When a patient gets a biosimilar instead of the original biologic drug, they shouldn’t expect any difference in safety. But here’s the catch: biosimilars aren’t copies like generic pills. They’re made from living cells, and even tiny changes in the manufacturing process can affect how the body reacts. That’s why adverse event monitoring for biosimilars isn’t just important-it’s a complex, high-stakes system designed to catch problems before they spread.
Why Biosimilars Need Special Safety Tracking
Unlike small-molecule generics, which are chemically identical to their brand-name counterparts, biosimilars are highly similar-but not identical-to the original biologic. This isn’t a flaw; it’s biology. Biologics are large, complex proteins made in living cells. Two batches from the same manufacturer can vary slightly. Now imagine two different companies making versions of the same drug using different cell lines, purification methods, or storage conditions. Even if both meet regulatory standards, subtle differences might show up later in how patients respond. The biggest concern? Immunogenicity. That’s when the body sees the drug as foreign and mounts an immune response. It can lead to reduced effectiveness, allergic reactions, or even dangerous conditions like neutralizing antibodies that attack the patient’s own natural proteins. A patient on a biosimilar for rheumatoid arthritis might start feeling worse-not because the drug stopped working, but because their immune system started fighting it. This is why regulators didn’t just apply the same rules used for generics. They built new systems from the ground up.How Adverse Events Are Reported Around the World
Every country has its own way of collecting reports when something goes wrong. In the U.S., it’s the FDA’s FAERS system. In Europe, it’s EudraVigilance. Canada uses the Canada Vigilance Program. These systems rely on healthcare providers, patients, and drugmakers to report adverse events. But here’s the problem: most reports don’t say which version of the drug the patient got. In the U.S., a doctor might just write “adalimumab” without specifying if it was Humira or Amjevita. In 2022, only 12.7% of biologic adverse event reports in the U.S. included the exact biosimilar name, according to IQVIA data. That makes it nearly impossible to tell if a reaction came from the reference product or a biosimilar. That’s why some countries took stronger steps. Health Canada now requires that every adverse event report include the brand name and manufacturer. Spain started requiring biosimilar identification in electronic health records in 2020-and saw reporting accuracy jump from 58% to 92%. In the U.S., the FDA introduced four-letter suffixes in 2017 (like “-abp21” for Amjevita), but many providers still don’t use them. A 2022 survey found 63.4% of U.S. physicians were confused about how to document biosimilars correctly.The Role of Active Surveillance and Real-World Data
Spontaneous reporting-waiting for doctors to file reports-isn’t enough. It’s slow, inconsistent, and misses rare side effects. That’s why regulators turned to active surveillance. The FDA’s Sentinel Initiative scans millions of electronic health records, insurance claims, and pharmacy databases to find patterns. If a spike in liver enzyme elevations shows up among patients taking a specific biosimilar, the system flags it. Same with EMA’s VigiLyze, an AI tool launched in 2022 that analyzes 1.2 million new case reports every year with 92.4% accuracy. These systems don’t just look at structured data. They use natural language processing to dig into doctors’ notes, discharge summaries, and lab results. One hospital in Toronto started using AI to scan clinical notes for phrases like “rash after switch” or “no improvement since biosimilar.” Within six months, they identified three previously missed cases of antibody development. But it’s expensive. Building this kind of system costs between $250,000 and $500,000 for mid-sized companies. That’s why many rely on third-party vendors like ArisGlobal or Oracle Health Sciences, which handle the tech and compliance for a fee.
What’s in the Risk Management Plan?
Before a biosimilar even hits the market, the company must submit a Risk Management Plan (RMP). This isn’t a formality-it’s a living document that outlines exactly how they’ll track safety after approval. The RMP must include:- Specific plans for monitoring immunogenicity
- How they’ll distinguish their product from the reference drug in reports
- Plans for post-marketing studies if needed
- How they’ll train prescribers and pharmacists
Why Underreporting Is a Silent Crisis
Despite all the systems in place, most adverse events go unreported. In the U.S., biosimilars made up 8.7% of biologic prescriptions in 2021, but only 0.3% of adverse event reports came from biosimilars. That’s a massive gap. Why? Patients don’t know what they’re taking. Pharmacists often swap biosimilars without telling them. A 2022 Arthritis Foundation survey found 41.2% of patients on biosimilars couldn’t say whether they got the reference product or the biosimilar. Doctors don’t always know either. A 2021 study showed only 37.8% of U.S. pharmacists knew the exact details needed to report a biosimilar adverse event correctly. And when a patient says, “I got sick after my shot,” the doctor doesn’t always ask, “Was it Humira or Adalimumab?” This isn’t just a paperwork problem. It’s a safety problem. If we can’t tell which drug caused the reaction, we can’t fix it.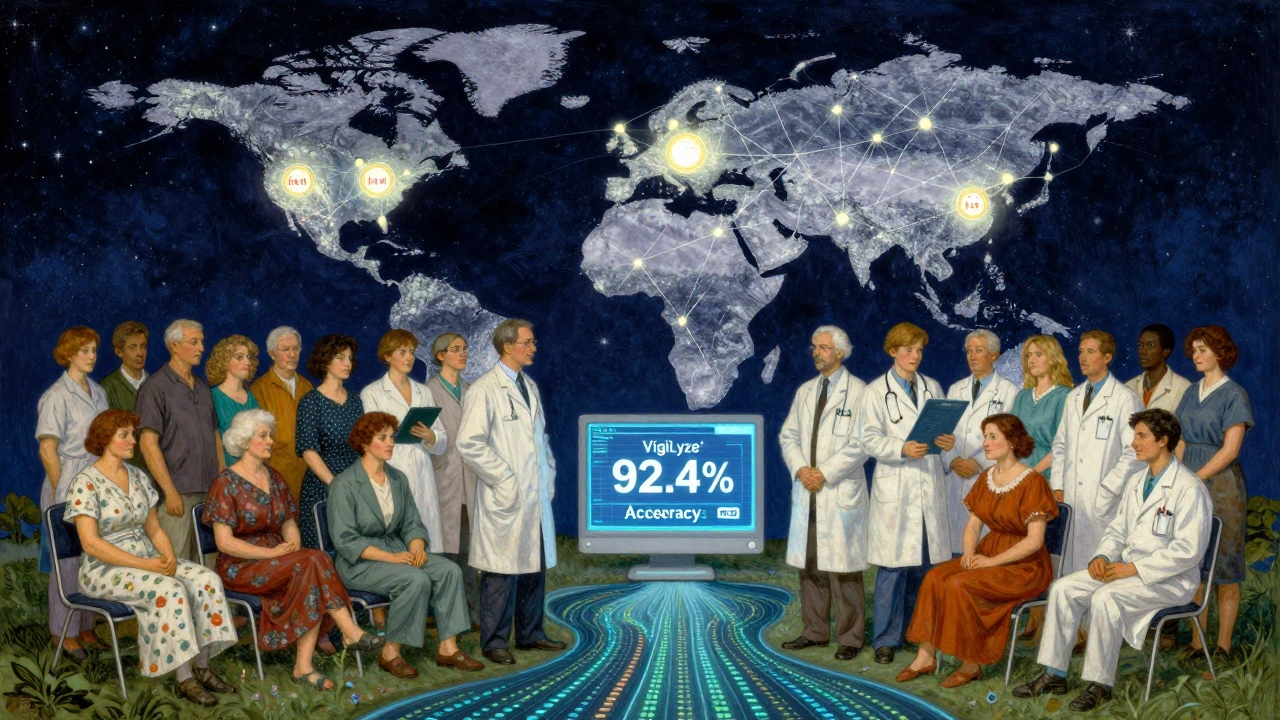
What’s Changing in 2025 and Beyond
The number of biosimilars is exploding. The global market is expected to hit $34.9 billion by 2028. More products mean more complexity. By 2030, WHO predicts over 300 biosimilars will be on the market, targeting just 30 reference drugs. That’s a nightmare for tracking. New solutions are coming. Health Canada’s 2023 rule requires manufacturers to clearly identify the product in every report-failure means fines up to $500,000 CAD. The WHO and ICH are pushing for a global unique identifier system for biologics by 2026, similar to barcodes on medical devices. Early trials in Switzerland showed this could cut attribution errors by 73.5%. AI will play a bigger role. Systems like VigiLyze are already using machine learning to predict which reports are most likely to signal a real safety issue. Soon, they’ll integrate with hospital systems to auto-flag changes in lab values or new symptoms after a biosimilar switch. But the real fix? Education. Patients need to know what they’re taking. Pharmacists need training. Doctors need better EHR templates. Without that, even the smartest tech won’t help.What Patients and Providers Can Do Today
You don’t need to wait for global systems to improve. Here’s what you can do right now:- Patients: Ask your pharmacist: “Is this the brand or the biosimilar? What’s the manufacturer?” Write it down. Keep a list of all your biologics and which version you got each time.
- Doctors: Always document the exact product name and manufacturer in the chart. Don’t just write “adalimumab.” Write “Amjevita (Amgen).”
- Pharmacists: When substituting, tell the patient. Give them a printed note. Update their medication list in the system.
- Everyone: Report any unusual side effect-even if you’re not sure which drug caused it. Every report counts.
Are biosimilars less safe than the original biologic drugs?
No. Regulatory agencies like the FDA, EMA, and Health Canada require biosimilars to show no clinically meaningful difference in safety, purity, or effectiveness compared to the reference product. Real-world data from Denmark, Canada, and the U.S. have consistently shown that biosimilars have similar safety profiles. The difference isn’t in safety-it’s in how we track it. Because biosimilars aren’t identical, we need better systems to detect rare differences, especially in immune reactions.
Why do biosimilars need unique names or suffixes?
Unique names-like the four-letter suffixes used in the U.S. (e.g., adalimumab-abp21)-help healthcare providers and regulators know exactly which product a patient received. Without them, adverse event reports get mixed up. If 10 different companies make versions of the same drug, and everyone just calls it “adalimumab,” there’s no way to tell if a reaction came from one company’s version or another. Suffixes make traceability possible.
Can biosimilars cause more immune reactions than the original drug?
There’s no strong evidence that biosimilars cause more immune reactions overall. But because they’re made differently, there’s a theoretical risk. Small changes in the manufacturing process can affect how the protein folds or what impurities remain. These could trigger immune responses in rare cases. That’s why pharmacovigilance systems focus heavily on immunogenicity monitoring. So far, large studies and real-world data haven’t shown a significant difference-but we’re still watching closely.
What happens if a biosimilar causes a serious side effect?
If a serious adverse event is reported and linked to a biosimilar, regulators investigate. The manufacturer must submit a detailed report within 15 days in the U.S. and Canada. If the signal is confirmed, the company may be asked to update the product label, run additional studies, or even pull the product. In rare cases, like with a 2019 case in Germany involving a biosimilar for multiple sclerosis, the product was temporarily restricted while investigations were underway. The system is designed to act fast-before more patients are affected.
Why aren’t all countries using the same biosimilar tracking system?
Regulatory systems are shaped by history, politics, and healthcare structure. The EU prioritizes efficiency and treats biosimilars as part of the same product family. The U.S. and Canada emphasize traceability and accountability, so they require stricter identification. There’s no global standard yet, but efforts are underway through the ICH and WHO to harmonize reporting formats, coding systems (like MedDRA), and risk management requirements. Full alignment is expected by 2027-2030.
How can I report an adverse event from a biosimilar?
In the U.S., report to the FDA through MedWatch: www.fda.gov/medwatch. In Canada, use Health Canada’s Canada Vigilance Online Reporting. In the EU, contact your national authority. Always include: the drug name (brand and manufacturer), batch/lot number if known, your symptoms, when they started, and whether you switched from the reference product. Even partial information helps.


Comments(10)