Azathioprine Monitoring Schedule Calculator
This calculator helps you track your azathioprine monitoring schedule based on FDA and medical guidelines. Blood tests are critical for early detection of potential side effects like aplastic anemia.
azathioprine is a common immunosuppressant, but a rare side effect-aplastic anemia-can be life‑changing. This guide breaks down what you need to know, from how the drug works to warning signs and what to do if trouble starts.
Key Takeaways
- Azathioprine is used for autoimmune diseases and organ‑transplant maintenance.
- Aplastic anemia is a rare but serious bone‑marrow failure that can be triggered by the drug.
- Incidence is roughly 0.5 cases per 10,000 patients, higher in those with genetic TPMT deficiency.
- Regular blood‑count monitoring can catch problems early.
- If aplastic anemia develops, stopping the drug and starting hematology care is critical.
What Is Azathioprine?
Azathioprine is a synthetic purine analog that suppresses the immune system by interfering with DNA synthesis in rapidly dividing cells. It was first approved by the FDA in 1968 and is prescribed for conditions like rheumatoid arthritis, inflammatory bowel disease, and to prevent organ‑reject rejection after transplants.
How Azathioprine Works
The drug converts inside the body to 6‑mercaptopurine, which blocks the production of purine nucleotides. Without enough nucleotides, immune cells can’t proliferate, dampening the overactive immune response that drives many chronic illnesses.
Understanding Aplastic Anemia
Aplastic anemia is a condition where the bone marrow stops making enough new blood cells-red cells, white cells, and platelets. The result is fatigue, easy bruising, infections, and sometimes life‑threatening bleeding. While many causes exist (viral infections, chemicals, radiation), drug‑induced cases are a small but recognized fraction.
The Link Between Azathioprine and Aplastic Anemia
Large pharmacovigilance databases (e.g., FDA’s AERS) report an incidence of about 0.5‑1 case per 10,000 azathioprine users. A 2022 retrospective cohort study of 35,000 patients showed that the risk spikes in the first six months of therapy, especially in people with low or absent thiopurine methyltransferase (TPMT) activity.
Mechanistically, the drug’s impact on DNA synthesis can unintentionally target hematopoietic stem cells, leading to pancytopenia if the marrow cannot recover.
Who Is More Likely to Develop This Side Effect?
- TPMT deficiency: Individuals lacking the TPMT enzyme process the drug more aggressively, raising toxic metabolite levels.
- Older adults (over65) because bone‑marrow reserves naturally decline.
- Patients on high cumulative doses (>3g per year).
- Concurrent use of other marrow‑suppressing drugs (e.g., cyclophosphamide).
Warning Signs to Watch For
Since early symptoms mimic common ailments, staying alert is crucial. Look for:
- Unexplained fatigue or shortness of breath.
- Frequent nosebleeds or gum bleeding.
- Bruising from minor bumps.
- Recurring infections (e.g., sinusitis, urinary‑tract infections).
- Pale skin or yellowish tint (signs of low red‑cell count).
If any of these appear, contact your doctor immediately for a complete blood count (CBC).
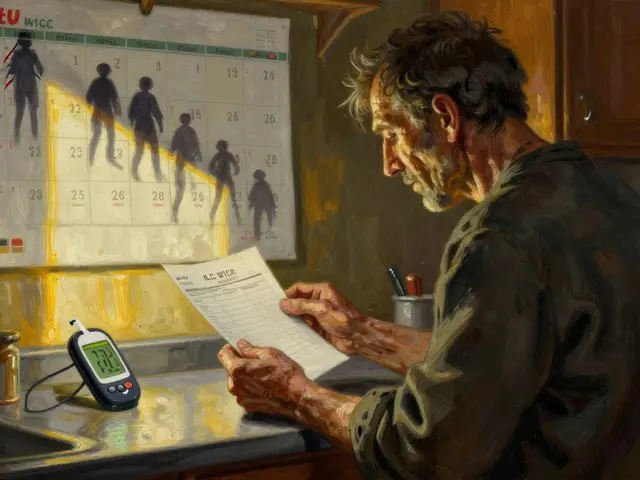
Monitoring & Prevention Strategies
Doctors typically follow a monitoring schedule that looks like this:
- Baseline CBC and liver‑function tests before starting azathioprine.
- Weekly CBC for the first month.
- Bi‑weekly CBC for months2‑3.
- Monthly CBC thereafter, unless abnormalities arise.
Testing for TPMT activity before the first dose can cut the risk dramatically-patients with low activity are often started on a reduced dose or switched to a different medication.
What to Do If Aplastic Anemia Is Diagnosed
Immediate steps include:
- Discontinuing azathioprine.
- Referral to a hematologist.
- Supportive care: blood transfusions, platelet infusions, and infection‑prophylaxis antibiotics.
- Potential therapies: antithymocyte globulin (ATG) plus cyclosporine, or hematopoietic stem‑cell transplant for severe cases.
Recovery timelines vary. Some patients regain normal counts after drug withdrawal, while others need long‑term immunosuppression.

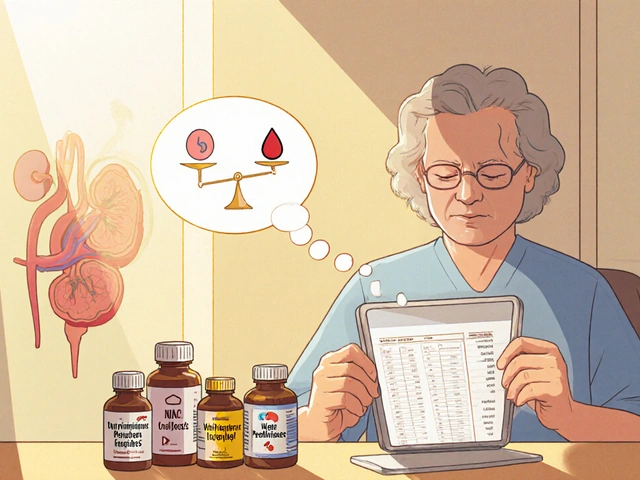
Alternative Immunosuppressants with Lower Aplastic Anemia Risk
When azathioprine poses too much risk, clinicians may consider:
- Mycophenolate mofetil - inhibits a different enzyme (IMP dehydrogenase) and shows a 0.1 case per 10,000 patients.
- Methotrexate - widely used in rheumatology, with aplastic anemia reported in fewer than 1 in 100,000 patients.
- Cyclosporine - primarily works on T‑cell activation, rarely linked to marrow failure.
Choosing an alternative depends on the underlying disease, patient age, kidney function, and previous drug tolerance.
Comparison of Aplastic Anemia Incidence Across Common Immunosuppressants
| Drug | Incidence | Typical Monitoring Frequency |
|---|---|---|
| Azathioprine | 0.5‑1 | Weekly → Monthly CBC |
| Mycophenolate mofetil | 0.1 | Monthly CBC |
| Methotrexate | 0.02 | Every 2‑4weeks CBC |
| Cyclophosphamide | 0.03 | Every 1‑2weeks CBC |
Practical Tips for Patients on Azathioprine
- Ask your doctor for a TPMT test before the first dose.
- Keep a symptom diary-note any bruising, bleeding, or infections.
- Never skip scheduled blood tests; they are the earliest alarm.
- If you start another medication (e.g., antibiotics), tell your clinician-some drugs raise azathioprine levels.
- Stay hydrated and maintain a balanced diet; proper nutrition supports bone‑marrow health.
Frequently Asked Questions
How soon after starting azathioprine can aplastic anemia appear?
Most cases surface within the first six months, but delayed presentations up to a year have been documented. Early monitoring is therefore essential.
Can the effect be reversed if caught early?
If the drug is stopped promptly and the marrow isn’t severely damaged, blood counts often recover over weeks to months. Severe cases may require immunosuppressive therapy or stem‑cell transplant.
Is TPMT testing mandatory?
Guidelines from major gastroenterology societies recommend TPMT screening before initiating azathioprine. It isn’t legally required, but it dramatically cuts the risk of marrow toxicity.
What other side effects should I be aware of?
Common issues include nausea, liver‑enzyme elevations, and increased infection risk. Rarely, patients develop pancreatitis or skin cancers after long‑term use.
Should I stop azathioprine if I feel fine?
Never stop or adjust the dose on your own. Even when you feel well, the drug continues to affect bone‑marrow cells. Always discuss changes with your prescriber.





Comments(11)