Most people don’t realize that a pill they take for anxiety or sleep could be quietly stealing their memory and making them more likely to break a hip. Benzodiazepines-drugs like Valium, Xanax, and Ativan-are among the most commonly prescribed medications in the world. But for every person who finds relief, another is at risk of something far more dangerous: long-term brain fog, unexplained falls, and a withdrawal process that can feel like losing your mind.
How Benzodiazepines Change Your Brain
Benzodiazepines work by boosting GABA, the brain’s main calming chemical. That’s why they work so well for panic attacks or insomnia. But this same mechanism slows down the parts of your brain responsible for forming new memories and coordinating movement. Within hours of taking even a single dose, you might notice you forget where you put your keys or feel unsteady on your feet. These aren’t side effects you’ll outgrow-they’re signs the drug is already affecting your brain.
Studies show benzodiazepines hit the hippocampus hardest-the area that turns short-term experiences into lasting memories. A 2023 meta-analysis of 19 studies found that people taking these drugs had measurable declines in recent memory, processing speed, and attention. The effects weren’t small. On average, users scored 10 to 15 points lower on IQ tests compared to non-users. That’s the difference between remembering your grandchild’s birthday and forgetting it entirely.
The Hidden Cost: Memory Loss That Doesn’t Go Away
Many assume that once you stop taking benzodiazepines, your memory bounces back. That’s not true for most people. Research tracking users for up to 10 months after quitting found that only 45% returned to normal cognitive function. The rest kept struggling with brain fog, trouble focusing, and memory gaps-even after months of being off the drug.
It’s not just about forgetting names. People report losing track of conversations, forgetting appointments they just made, or walking into a room and not knowing why. One 72-year-old woman in Wellington told her doctor she’d stopped recognizing her own photos. She’d been on diazepam for 12 years. After tapering, it took her 14 months to feel like herself again.
Neuroimaging doesn’t show brain damage-no shrunk areas or lesions. Instead, it shows the brain is working harder to do the same tasks. Your neurons are scrambling to compensate. That’s why recovery is slow: your brain has to rewire itself, one connection at a time.
Falls Aren’t Just Accidents-They’re a Side Effect
Every year in the U.S., about 93,000 older adults end up in the emergency room because of a fall linked to benzodiazepines. In New Zealand, where one in five people is over 65, the numbers are rising too. The risk isn’t just higher-it’s predictable.
Benzodiazepines reduce balance by 30-40% and slow reaction times by 25-35%. That means if you trip on a rug, your body doesn’t catch itself fast enough. If you stand up too quickly, your blood pressure drops and you black out for a second. High-potency drugs like alprazolam (Xanax) are especially dangerous: they carry a 60% higher fall risk than older, longer-acting ones like diazepam.
The American Geriatrics Society has listed benzodiazepines as inappropriate for older adults since 2012. Yet they’re still prescribed. Why? Because doctors often don’t know the alternatives-or patients are too anxious to ask for them.

Tapering Isn’t Optional-It’s Essential
If you’ve been on benzodiazepines for more than a few weeks, stopping cold turkey is dangerous. Seizures, hallucinations, and extreme anxiety can follow. But tapering too fast can make things worse. That’s why the Ashton Protocol is still the gold standard.
Here’s how it works: you switch from your current benzodiazepine to diazepam (Valium), because it has a long half-life and smooths out withdrawal. Then, you reduce your dose by 5-10% every 1-2 weeks. For someone on a high dose for 10+ years, that could mean a taper lasting 6 to 12 months.
A 2021 study of 312 long-term users showed that following this method led to a 68.5% success rate at six months. People who tapered slowly reported fewer withdrawal symptoms and clearer thinking within weeks. One man in his 60s cut his dose by 2.5% every three weeks. By month four, he could read a book without losing his place. By month eight, he was walking his dog without fear of falling.
But here’s the catch: 22% of people needed to pause their taper for weeks because symptoms flared up. And 8% couldn’t continue at all. That’s why support matters. Joining a community like the Benzodiazepine Information Coalition helps. People there share tips: use apps like BrainBaseline to track memory changes, keep a journal, and never rush.
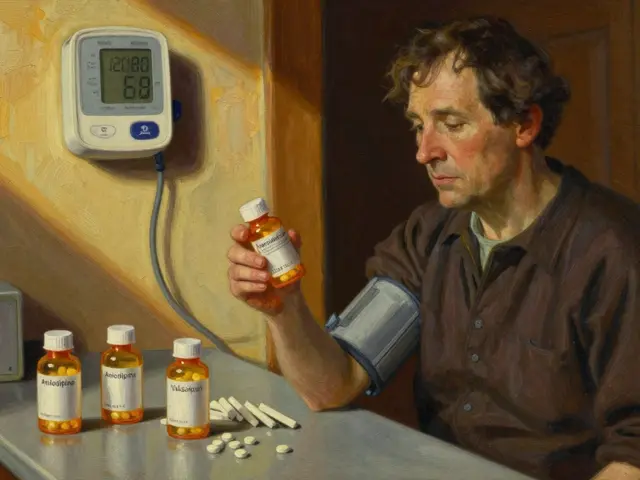
What to Do If You’re on Benzodiazepines
If you’re taking one of these drugs, here’s what to do now:
- Don’t stop suddenly. Talk to your doctor about switching to diazepam if you’re on a short-acting drug.
- Ask for a cognitive baseline test-MMSE or MoCA. Do it again in six months.
- If your score drops by 2 points (MMSE) or 3 points (MoCA), discuss stopping.
- Set a taper goal. Even reducing your dose by 5% in three months is progress.
- Track your symptoms. Note brain fog, balance issues, or sleep changes. Write them down. You’ll need this later.
For older adults, the maximum safe daily dose is 5 mg of diazepam. For anyone under 65, it’s 10 mg. Many people are on far more than that-sometimes for years.

The Future: Better Options Are Coming
There’s hope. New drugs are being tested that target only the anxiety parts of the brain, not the memory or balance centers. Early trials of α2/α3-selective agonists show 70% reduction in anxiety with no memory loss. These aren’t available yet, but they’re in phase II trials-and they’re the reason researchers are finally turning away from old benzodiazepines.
In the meantime, non-drug options work better than most people think. CBT for anxiety, sleep restriction therapy for insomnia, and regular strength training (yes, lifting weights) all reduce anxiety and improve balance without a single pill.
It’s Not Weakness-It’s Wisdom to Quit
Some people feel guilty for wanting to stop. They think they’re failing if they can’t handle life without a pill. But the real failure is staying on a drug that steals your memory, makes you fall, and keeps you dependent for years.
One woman in her 70s told me, “I thought I needed Xanax to live. Turns out, I needed to live to get off Xanax.” She tapered over 10 months. Now she gardens, travels, and remembers her grandchildren’s names.
You don’t have to be perfect. You don’t have to quit tomorrow. But if you’re on benzodiazepines, you owe it to yourself to learn the risks-and take the next step.
Can benzodiazepines cause permanent memory loss?
Benzodiazepines don’t cause permanent structural brain damage, but they can lead to long-lasting cognitive impairment. Studies show that after stopping, about 55% of long-term users still have measurable deficits in memory, attention, and processing speed for months or even years. These aren’t always fully reversible, especially if the drug was taken for over a decade. The brain can recover, but it takes time-and not everyone gets back to where they started.
Why is diazepam used for tapering instead of other benzodiazepines?
Diazepam has a very long half-life-up to 100 hours-which means it clears slowly from the body. This creates a smoother withdrawal with fewer spikes in anxiety or insomnia. Short-acting drugs like alprazolam or lorazepam leave the system quickly, causing intense rebound symptoms between doses. Switching to diazepam reduces these fluctuations, making the taper more manageable and safer.
How long does it take to recover cognitively after stopping benzodiazepines?
Recovery varies. Some people notice improvement in processing speed and focus within 4-8 weeks of starting a slow taper. But full cognitive recovery often takes 6 to 18 months. Memory and attention can linger longer. A 2023 study found that even after 10 months off the drug, nearly half of users still had below-average scores on memory tests. Patience and consistent healthy habits-sleep, exercise, and mental stimulation-are key.
Are there safer alternatives to benzodiazepines for anxiety or insomnia?
Yes. For anxiety, cognitive behavioral therapy (CBT) is as effective as medication and has no side effects. For insomnia, sleep restriction therapy and stimulus control are proven methods. Non-benzodiazepine sleep aids like trazodone or melatonin receptor agonists (ramelteon) are safer for long-term use. Antidepressants like SSRIs are first-line for chronic anxiety. Physical activity, mindfulness, and reducing caffeine also help significantly.
Should older adults ever take benzodiazepines?
The American Geriatrics Society and European guidelines recommend avoiding them entirely in adults over 65. The risks-falls, fractures, confusion, and accelerated cognitive decline-far outweigh the benefits. If absolutely necessary, use the lowest possible dose for the shortest time-no longer than 2-4 weeks. Always screen for cognitive changes every six months. There are safer, more effective options for seniors.
What should I do if I feel worse during tapering?
Feeling worse is common-but it doesn’t mean you should go back to your old dose. Withdrawal symptoms often peak around weeks 2-4 of tapering. If symptoms are severe, pause the taper for 2-4 weeks at your current dose. Then resume with smaller reductions (2-3% instead of 5-10%). Keep a symptom journal. Talk to a doctor who understands benzodiazepine withdrawal. Support groups can also help you stay on track without feeling alone.




Comments(13)