Every year in the U.S., more than 1.3 million people are injured and over 7,000 die because of medication errors. These aren’t random accidents. They’re preventable. And they happen because systems fail, not because providers are careless. The truth is, even the most experienced nurse or doctor can make a mistake when the tools around them are outdated, overwhelming, or poorly designed. Medication safety isn’t just about double-checking prescriptions-it’s about building a culture where errors are caught before they reach the patient.
Why Medication Safety Can’t Be an Afterthought
Medication errors don’t start with a nurse giving the wrong dose. They start with a handwritten script, a mislabeled vial, a defaulted field in an EHR, or an alert that’s been ignored so many times it’s background noise. The World Health Organization calls this a global crisis. Their Medication Without Harm initiative, launched in 2017, aimed to cut severe, avoidable harm by 50% in five years. By 2022, progress was real-but uneven. Hospitals that used all 12 ISMP Targeted Best Practices saw 63% fewer serious errors. Those that didn’t? They kept losing patients to preventable mistakes.The Five Rights Are Just the Starting Point
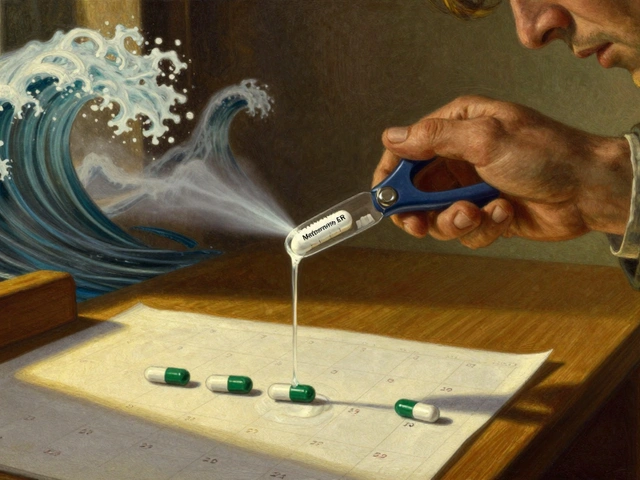
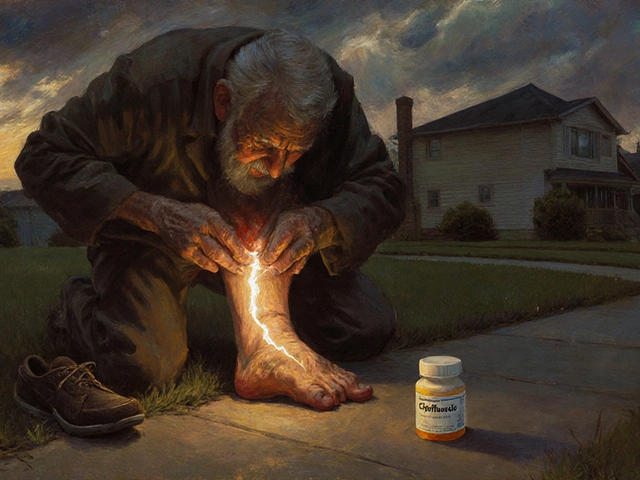
You’ve heard them: right patient, right drug, right dose, right route, right time. But in today’s fast-paced clinics and ERs, checking those boxes isn’t enough. High-alert medications like IV oxytocin, insulin, or methotrexate can kill in minutes if given wrong. A single typo-typing daily instead of weekly for methotrexate-has led to fatal overdoses. That’s why systems now require a hard stop: no order goes through unless the provider confirms the correct indication. No exceptions.Barcode Scanning Isn’t Optional-It’s the New Standard
Barcode-assisted medication administration (BCMA) isn’t a luxury. It’s a lifeline. When nurses scan the patient’s wristband and the medication’s barcode before giving a drug, errors drop by 41.1%. That’s not theory-it’s data from the Institute for Healthcare Improvement. But here’s the catch: 30% of nurses still bypass the system during emergencies. Why? Because the scanner is slow, the battery dies, or the system locks up. That’s not negligence-it’s a design flaw. The fix? Make BCMA seamless. Train staff on workarounds that don’t compromise safety. And never punish someone for reporting a broken system.Electronic Prescribing Works-If It’s Done Right
Handwritten prescriptions are a relic. They cause 25% more errors than e-prescriptions. But even digital systems aren’t perfect. A 2022 study in the New England Journal of Medicine found community pharmacies still had a 2.3% error rate after switching to e-prescribing. Why? Workflow disruptions. A doctor sends a script, the pharmacy’s system doesn’t recognize the dosage format, and the pharmacist has to call back. That delay leads to rushed decisions. The solution? Standardize formats across EHRs. Require exact units (mg, not “Mg”). Force confirmation of dose ranges. And never let a system auto-fill a dose without human review.
Alert Fatigue Is Killing More Than Patients
Clinical decision support systems are supposed to protect you. But if your EHR throws 25 alerts per patient visit, and 90% of them are irrelevant, you stop listening. Studies show clinicians override 49% to 96% of alerts. One nurse on Reddit said she ignores 80% because they’re “noise.” That’s not laziness-it’s burnout. The fix isn’t fewer alerts. It’s smarter alerts. AI-powered systems now identify which alerts matter most. One 2023 study in Nature Medicine showed AI could predict 89% of potential prescribing errors before they happened-compared to 67% for traditional systems. The future isn’t more noise. It’s better signal.Training Isn’t a One-Time Event
You wouldn’t let a pilot fly without annual simulator training. Why do we expect nurses and doctors to stay sharp on medication safety with a single 2-hour lecture? The Agency for Healthcare Research and Quality recommends 16-24 hours of initial training, followed by 8 hours of annual refresher courses-with simulations. Real-life scenarios. Mock code blues. Wrong-dose drills. At Johns Hopkins, embedding pharmacists in ICUs cut medication errors by 81%. Why? Because safety isn’t a policy-it’s a practice. And practice requires repetition, feedback, and accountability.High-Performing Teams Have a Different Culture
The best hospitals don’t just have better tech-they have better teams. They use the AHRQ Hospital Survey on Patient Safety Culture. Top performers score in the 75th percentile or higher on “organizational learning” and “teamwork across units.” That means if a nurse spots a potential error, she doesn’t fear being blamed-she’s encouraged to speak up. That’s the power of a nonpunitive reporting culture. Dr. Tejal Gandhi of the National Patient Safety Foundation says transparency isn’t optional-it’s the foundation of learning. When errors are reported without fear, systems improve. When they’re hidden, patients pay the price.
Technology Alone Won’t Save You
EHRs were supposed to fix everything. Instead, they created new problems. Dr. David Bates’ research at Brigham and Women’s found 34% of digital medication errors came from dropdown menus and default values. A doctor selects “Lantus” from a list, but the system auto-fills a 20-unit dose when the patient only needs 10. No one notices because the default looks normal. The FDA logged 214 adverse events tied to EHR usability in 2022-up 37% from 2021. The lesson? Technology must be designed for humans, not the other way around. Test systems with frontline staff. Watch them use it. Fix the friction.What You Can Do Today
You don’t need a $1 million system to start improving safety. Here’s what works right now:- Review your top 5 high-alert medications. Are they labeled clearly? Are dose limits built into your EHR?
- Run a mock BCMA drill. How many staff can complete it without bypassing the system?
- Survey your team: How many alerts do you override weekly? Why?
- Implement a 5-minute daily safety huddle. One question: “What’s one thing that could go wrong today?”
- Update your medication policy. If it hasn’t changed in 3 years, it’s outdated. Use ASHP’s 2022 guidelines as your baseline.
The Future Is AI-But Humans Still Hold the Keys
AI is changing medication safety. Algorithms now flag errors before they’re typed. Some systems can cross-reference a patient’s lab results, allergies, and current meds to suggest safer alternatives. But AI doesn’t replace judgment-it supports it. The FDA warns that over-reliance on tech is dangerous. The most effective systems combine AI predictions with human verification. In 2024, ISMP added new guidelines for AI-assisted prescribing. The message is clear: Use the tools. But never stop asking, “Does this make sense for this patient?”Final Thought: Safety Is a Habit, Not a Policy
Medication safety isn’t about compliance. It’s about care. It’s about looking a patient in the eye and knowing you did everything possible to keep them safe. That means fixing broken systems. Speaking up when something feels off. Training relentlessly. And never accepting “that’s how we’ve always done it” as an excuse. The data is clear: When providers are trained, supported, and empowered, errors drop. Patients live. And that’s the only metric that matters.What are the most common causes of medication errors in hospitals?
The top causes include miscommunication during handoffs, illegible handwriting on paper prescriptions, incorrect dose selection in EHRs due to default values, failure to scan barcodes, and alert fatigue leading to ignored warnings. High-alert medications like insulin, opioids, and IV potassium are especially risky when protocols aren’t followed.
How effective is barcode scanning in reducing medication errors?
Barcode-assisted medication administration (BCMA) reduces administration errors by 41.1%, according to the Institute for Healthcare Improvement. When combined with electronic prescribing and clinical decision support, error rates can drop from 5.9 per 100 orders to as low as 1.2 per 100 orders within 18 months.
What is alert fatigue, and why is it dangerous?
Alert fatigue occurs when clinicians are overwhelmed by too many clinical decision support alerts-often more than 20 per patient encounter. Studies show 49% to 96% of these alerts are overridden because they’re irrelevant or repetitive. This desensitization means real warnings get ignored, putting patients at risk.
How much training do healthcare providers need for medication safety?
The AHRQ recommends 16-24 hours of initial training for new clinicians, with simulation-based learning. Annual refresher training should be at least 8 hours and include real-world scenarios, not just online modules. Top-performing hospitals embed pharmacists in units and conduct weekly safety drills.
What role does AI play in modern medication safety?
AI is now used to predict prescribing errors before they occur. One 2023 study in Nature Medicine found AI algorithms detected 89% of potential errors, compared to 67% with traditional systems. AI doesn’t replace human judgment-it prioritizes the most critical alerts and flags high-risk combinations based on patient history, lab results, and drug interactions.
Are electronic health records making medication safety better or worse?
EHRs reduce errors from handwritten prescriptions by 48%, but they introduce new risks. A 2021 study found 34% of digital errors came from default values, dropdown menus, and poorly designed interfaces. The key is usability: EHRs must be tested with frontline staff and updated regularly to prevent workflow disruptions.
What are high-alert medications, and why do they need special handling?
High-alert medications-like IV insulin, oxytocin, morphine, and methotrexate-carry a high risk of causing serious harm if used incorrectly. Even small errors can be fatal. They require special protocols: hard stops in EHRs, double-checks by two staff members, clear labeling, and restricted access. ISMP lists these drugs as top priorities for safety interventions.
How can small clinics improve medication safety without big budgets?
Start with the basics: use free drug reference apps like Lexicomp or Epocrates, implement a two-person verification for high-alert drugs, create a simple error-reporting system without blame, and hold monthly safety huddles. Update policies using ASHP’s 2022 guidelines. Even small changes-like standardizing dose formats-can reduce errors significantly.




Comments(13)