Heartburn doesn’t just steal your sleep; it takes over your day. If you’ve spent nights propped up with pillows, sipping questionable remedies at 2 a.m., or ducking out of meals to find antacids, you know the drill. Here’s the kicker: nearly 60 million Americans wrestle with heartburn at least once a month, and for many, quick fixes aren’t enough. That’s where a medication like Prevacid steps in—designed for folks who need more than just an occasional chewable tablet to find real relief.
What is Prevacid and How Does it Work?
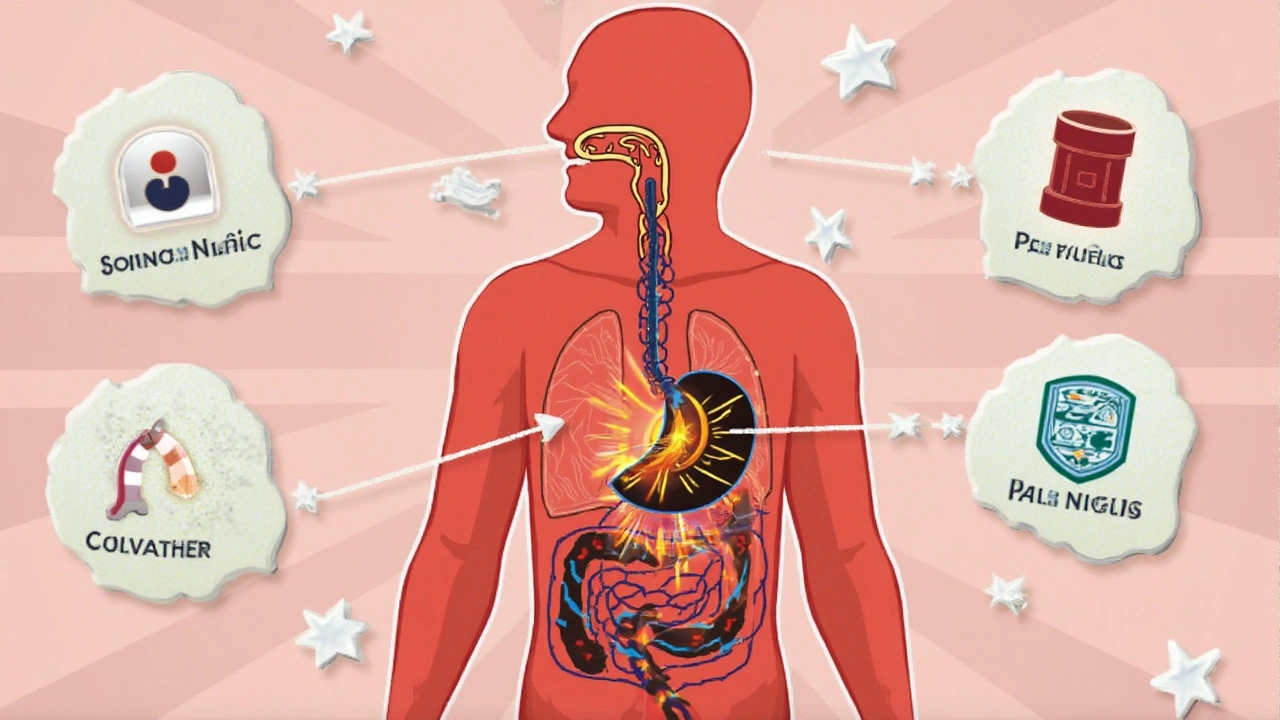
Prevacid is the brand name for lansoprazole, a type of medicine called a proton pump inhibitor (PPI). Its job is to block the pumps in your stomach lining that produce acid, cutting down on the burning, gnawing pain you get with acid reflux or ulcers. And it doesn’t just ease the symptoms—over time, it helps your esophagus and stomach heal from all that acid damage.
Doctors usually pull Prevacid out of their toolkit for these reasons:
- Persistent heartburn (the kind that shows up more than twice a week)
- Gastroesophageal reflux disease (GERD), which is just the medical way of saying nasty, stubborn acid reflux
- Stomach or duodenal ulcers
- Damage to the esophagus caused by years of reflux
- Infection with H. pylori (a common stomach bug that causes ulcers)
- Conditions like Zollinger-Ellison syndrome, where your stomach churns out more acid than it should
Prevacid isn’t the only PPI out there—omeprazole (Prilosec) and esomeprazole (Nexium) are cousins—but it’s been trusted since the FDA gave it a green light back in 1995. If you like data, here’s a quick comparison that shows why people reach for these meds:
| Medicine | Time to Symptom Relief (Typical) | How Long It Lasts | Common Dosing |
|---|---|---|---|
| Prevacid (Lansoprazole) | 1-4 days | 24 hours | 15-30 mg daily |
| Prilosec (Omeprazole) | 1-4 days | 24 hours | 20-40 mg daily |
| Nexium (Esomeprazole) | 1-4 days | 24 hours | 20-40 mg daily |
All three take a few days to really kick in, so don’t expect instant relief. The main advantage with Prevacid? Some people find it easier to take long-term, as its side effects profile is slightly milder for certain users, though every body reacts differently.
Common Uses and How to Take Prevacid
Prevacid comes in capsules, orally disintegrating tablets (the kind that dissolve on your tongue), and even as a powder for liquid. The standard over-the-counter dose is 15 mg, but doctors might prescribe the 30 mg strength for stubborn cases.
So, how do you actually take it? Here are the basics:
- Take Prevacid about 30 minutes before a meal. Most folks choose breakfast, but stick to the same meal every day.
- Swallow the capsule whole—don’t crush or chew it. If you hate pills, open the capsule and sprinkle its contents on a spoonful of applesauce or yogurt (ask your pharmacist how, just to be sure you get it right).
- For the dissolvable kind, just let it melt on your tongue and swallow. No water needed.
- If you’re doing liquid doses, measure carefully with the tool that comes in the box, not a kitchen spoon (accuracy matters here).
A lot of folks wonder: how long do I need to take Prevacid? For simple heartburn, a 14-day course is usually enough, but if you’ve got ulcers or tough GERD, it’s more like 4 to 8 weeks—and some people need maintenance doses for months. Your doc will decide what fits your case best.
Don’t double up if you miss a dose. Skip it and just take the next one on schedule. Overdoing it doesn’t fix things faster and just increases side effects.
If you’re on other meds—like blood thinners, anti-seizure drugs, or HIV meds—always check with your healthcare provider. Prevacid can mess with how these drugs work.
Prevacid Side Effects and Safety Concerns
Here’s where most people get nervous: side effects. The good news? For many, Prevacid is a breeze to tolerate. Still, you might notice things like:
- Headache (the most common, usually mild)
- Stomach pain or slight nausea
- Diarrhea or constipation
- Dizziness or mild fatigue
But let’s get real. There are some rare, but important, long-term risks you shouldn’t ignore:
- Low magnesium, which can cause muscle cramps or irregular heartbeats—more likely if you take PPIs for months
- Vitamin B12 deficiency (especially after a year or more of daily use)
- Fractures in older adults, mostly with high doses or long-term use
- Gut infections (PPIs slightly increase your risk for C. diff and a few other bugs that love low acid)
- Possible increased chance of kidney issues, though this is still under debate
If you experience severe tummy pain, persistent diarrhea, black stools, or sudden weakness after starting Prevacid, call your doctor. Some issues—like allergic reactions (hives, swelling, trouble breathing)—need emergency care. Don’t brush off anything that feels wrong.
Quit waiting for side effects to sneak up. Get simple blood tests every few months if you’re on Prevacid every day, especially for magnesium and kidney function. If you’re older or take lots of meds, check in sooner. Better safe than sorry.
Tips for Getting the Best Results with Prevacid
Here’s what separates folks who get relief from those who stay stuck with heartburn: smart habits. Taking Prevacid is only half the battle—the other half is changing up your routine.
- Stay Consistent. Swallow your Prevacid at the same time daily. It needs a routine to work its magic against stomach acid.
- Track Your Trigger Foods. Coffee, spicy peppers, garlic, chocolate, and soda—these are the usual suspects. If you spot patterns, adjust your eating habits.
- Lose the Tight Waistbands. Tight pants can squeeze your belly and make reflux worse. This is the rare case where sweatpants outshine jeans for medical reasons.
- Avoid Big Meals at Night. Late dinners can set you up for a night of burning misery. Aim for your final meal at least 3 hours before bed.
- Prop Up When Sleeping. Use a wedge pillow or raise your bed’s head by 6-8 inches. This trick keeps acid where it belongs while you sleep.
- Don’t Mix with Certain Drugs. Antifungals, anti-seizure meds, and even blood thinners can react badly with Prevacid. Double-check your list with a pharmacist or doctor.
- Limit Alcohol and Quit Smoking. Both mess with your lower esophageal sphincter and undo any good Prevacid is doing.
- Keep a Symptom Journal. Write down when you take Prevacid and when you feel pain or discomfort. It helps your doctor fine-tune your meds or spot patterns you missed.
For parents: if your child is prescribed Prevacid, make sure you’re giving the right dose for their age and weight. Ask questions, and don’t guess.
For pregnant or breastfeeding women, Prevacid is sometimes used if the benefits outweigh the risks. Talk it over with your OB-GYN or pediatrician first.
Notice any changes in how you feel? Don’t tough it out. Report it and don’t switch to another medication on your own.
What to Know About Drug Interactions and Warnings
Mixing Prevacid with other meds isn’t always safe. Here’s a handy rundown of interactions to watch for:
- Blood thinners (warfarin, clopidogrel): Prevacid can change how well they work, possibly making bleeding more likely.
- HIV meds (atazanavir, rilpivirine): Prevacid can lower their absorption, risking treatment failure.
- Digoxin (for heart problems): Prevacid may bump up digoxin levels, risking side effects.
- Methotrexate and some antifungals: Prevacid changes how your body handles these drugs.
- Iron supplements and some antibiotics (like ampicillin): Less stomach acid, less absorption, so these meds may not work as well.
When in doubt, run your medication list by your pharmacist. Even supplements and vitamins count. And watch out for over-the-counter meds that also fight acid—doubling up doesn’t help and might make things worse.
Certain people should be extra careful:
- Those with osteoporosis or high fracture risk, especially if using Prevacid for months
- Kidney or liver problems—dose adjustments may be needed
- People with a history of lupus—PPIs can sometimes trigger or worsen this
- Children—only use under a doctor’s close eye
Some folks try to get heartburn relief using antacids and Prevacid at the same time. Wait at least one hour after Prevacid before popping an antacid. The timing matters.
And don’t forget the number one rule: if your heartburn doesn’t improve in two weeks—or if it keeps coming back—see your doctor. Persistent heartburn can sometimes signal something more serious, like Barrett’s esophagus or even cancer.
Real-World Facts, Stats, and What Patients Say
People often ask, “Does Prevacid really work?” According to a review in the American Journal of Gastroenterology, about 80% of people with GERD feel better after a two-week course. For ulcers, the healing rate with Prevacid hits well over 85% after a month. Those are strong numbers.
But not everyone responds the same. Some report relief kicks in the first week, while others struggle with side effects or need their dose adjusted. If you’re one of the unlucky few who doesn’t get relief, don’t give up—there are other meds and solutions out there.
Prevacid also made headlines when studies a few years back linked long-term use to kidney problems and dementia. The kidney issue is real but rare, and mostly seen with years of high doses or when combined with other kidney-damaging drugs. The dementia connection? Not proven. So don’t let headlines scare you off, but use Prevacid smartly and stay in touch with your health team.
PPI use (like Prevacid) keeps climbing. In 2023, U.S. pharmacies filled over 80 million PPI prescriptions. That’s a lot of empty yogurt cups and breakfast routines changed forever!
Here’s what patients wish they knew at the start:
- “I thought it’d be instant. It took about 3 days before I woke up without that painful burn. Stick with it.”
- “I felt weirdly tired at first. After a week, that went away and I could eat without pain.”
- “Don’t make my mistake—talk to your doctor before mixing meds. I ended up dizzy from too much interaction.”
- “The dissolvable tablets make life easier if you can’t swallow pills. Tastes weird, but worth it.”
Prevacid works best as part of a larger plan—don’t just pop the pill and expect miracles. Listen to your body, stick to routines, and keep your doctor in the loop if anything changes. And if you’ve been up at night lately fighting that acid, maybe tonight’s the night you finally get the sleep you deserve.





Comments(17)