Immunosuppressant Drug Interactions – What You Need to Know
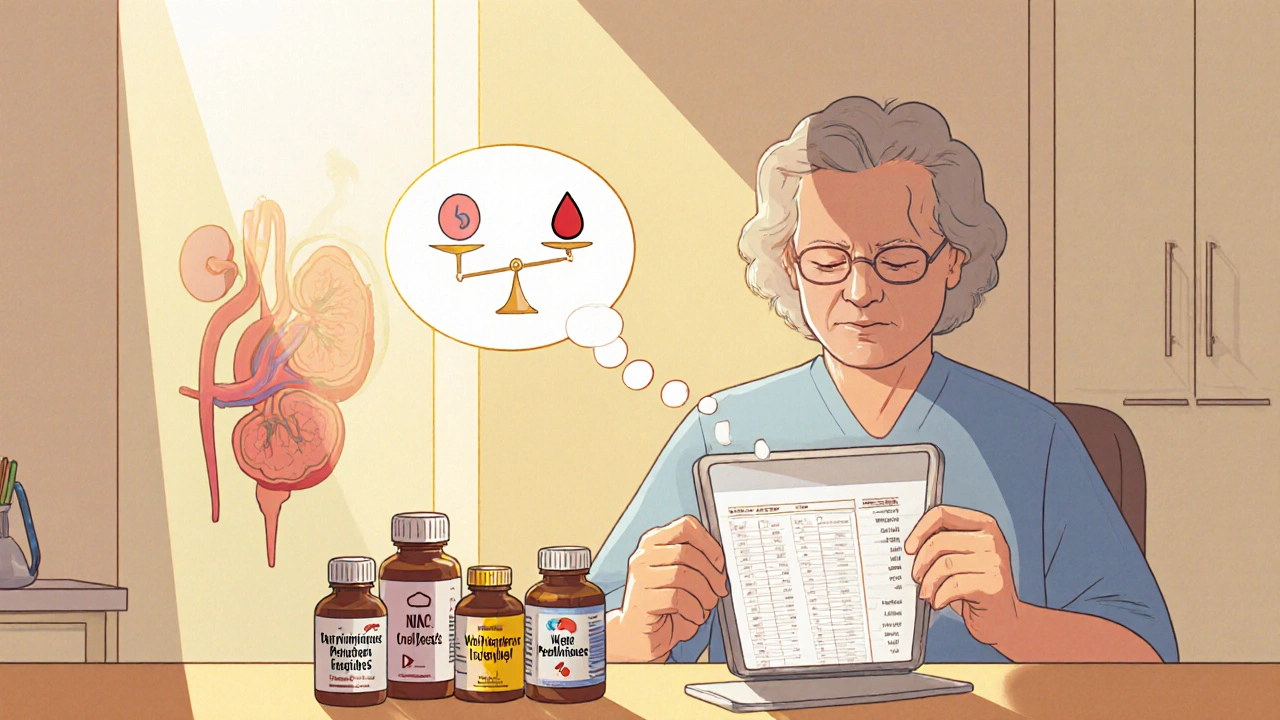
When dealing with immunosuppressant drug interactions, the combined effect of immune‑suppressing medicines and other substances can change how each drug works, leading to unwanted side effects or loss of effectiveness. Also known as immune suppressant interactions, this topic matters to anyone on a transplant regimen, autoimmune therapy, or long‑term steroid plan.
One of the most talked‑about drugs in this space is Azathioprine, a purine‑like immunosuppressant often prescribed after organ transplants or for conditions like rheumatoid arthritis. Azathioprine’s safety profile is closely tied to how the body processes it—especially via the CYP450 enzymes, a family of liver proteins that break down many prescription and over‑the‑counter medicines. When another drug blocks or speeds up these enzymes, azathioprine levels can swing dramatically, raising the risk of bone marrow toxicity or, conversely, losing its therapeutic punch.
Why should you care? The purpose of immunosuppressants is to keep the immune system from attacking a transplanted organ or misfiring in autoimmune disease. If a drug interaction pushes the dose too high, patients may face severe infections, liver damage, or even aplastic anemia, as highlighted in our Azathioprine article. If the dose falls too low, the body may reject the graft or flare the underlying disease, undoing months of treatment.
Typical culprits fall into a few familiar buckets. Antibiotics like clarithromycin or fluoroquinolones can inhibit CYP450, raising levels of drugs such as tacrolimus or cyclosporine. Antifungal agents (e.g., ketoconazole) and antivirals (especially protease inhibitors) have similar effects. Even common herbal supplements—St. John’s wort, ginseng, or grapefruit juice—can tilt the enzyme balance. Over‑the‑counter pain relievers, particularly NSAIDs, may worsen kidney strain when combined with calcineurin inhibitors. Recognizing these patterns lets clinicians and patients anticipate problems before they arise.
Patients fall into distinct groups, each with its own interaction profile. Transplant recipients often juggle multiple immunosuppressants, making enzyme‑driven swings especially risky. People with autoimmune disorders may be on a single agent like azathioprine, but they also frequently use steroids, NSAIDs, or disease‑specific biologics that add layers of complexity. Oncology patients receiving high‑dose regimens may encounter chemotherapy agents that share metabolic pathways, demanding extra vigilance.
Practical steps can keep you on the safe side. First, maintain an up‑to‑date medication list that includes prescription drugs, over‑the‑counter pills, vitamins, and herbal products. Share this list with every pharmacist and prescriber. Second, ask for baseline and periodic lab tests—complete blood counts, liver enzymes, and drug‑specific trough levels—to catch changes early. Third, never start a new supplement without checking its impact on CYP450; a quick chat with your doctor can prevent a costly dose adjustment later. Finally, use reputable sources—like our site’s detailed azathioprine guide—to understand warning signs such as unexplained bruising, fatigue, or jaundice.
Our collection of articles dives deep into these issues. You’ll find a clear breakdown of azathioprine’s bone‑marrow risks, a side‑by‑side look at how red yeast rice can mimic statins, and practical advice on buying safe generic medications online. By reading through the posts below, you’ll get a full picture of how specific drugs interact, what monitoring looks like, and which alternatives might be safer for your situation.
Ready to explore the details? Below you’ll discover a curated list of guides that unpack the most common and dangerous immunosuppressant drug interactions, offering real‑world tips you can apply right away.