Transplant Medication Management: What You Need to Know About Immunosuppressants and Side Effects
When you get a new organ, your body doesn’t know it’s supposed to accept it. That’s where transplant medication management, the ongoing process of taking drugs to prevent your immune system from attacking your transplanted organ. Also known as immunosuppressive therapy, it’s not a one-time fix—it’s a lifelong routine that keeps your transplant working. Without it, rejection can happen fast. Even a missed dose can trigger serious damage. This isn’t just about popping pills. It’s about understanding how these drugs interact with your body, your diet, and even other medicines you might be taking.
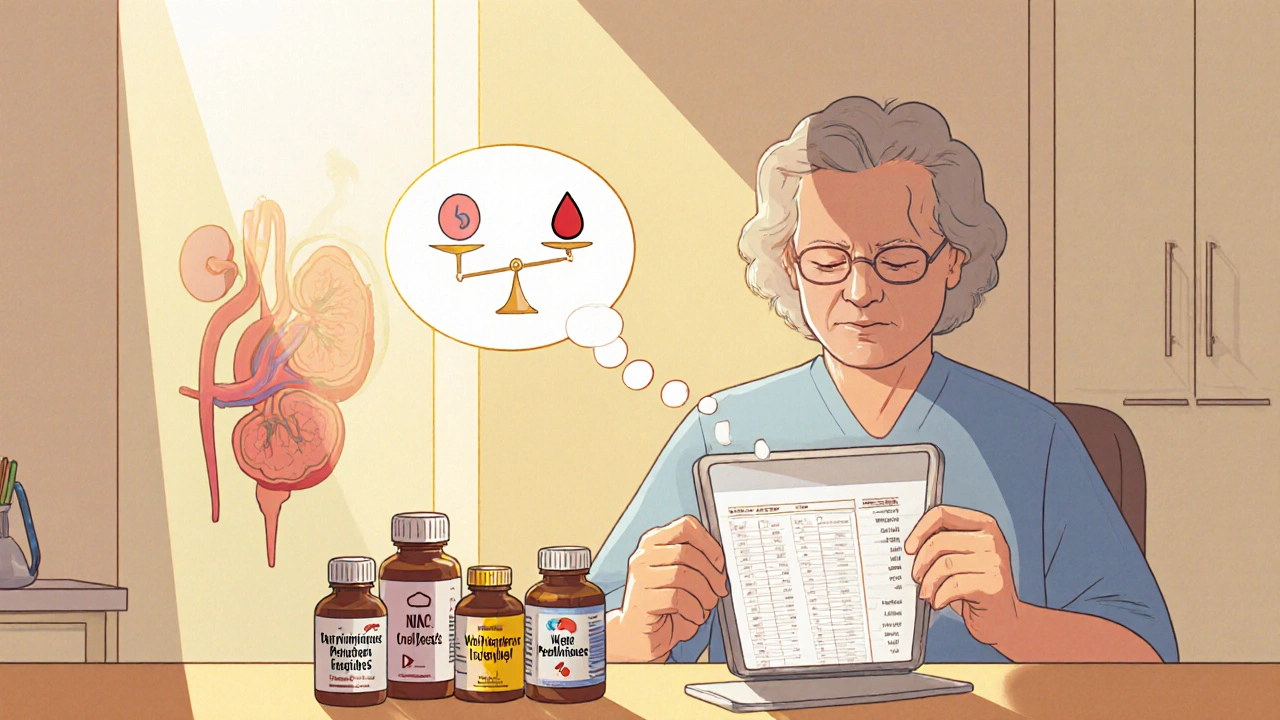
Immunosuppressants, a class of drugs designed to calm down your immune system so it doesn’t see your new organ as an invader. Also known as anti-rejection drugs, they include common names like tacrolimus, cyclosporine, and mycophenolate. Each one works differently, and your doctor picks the mix based on your organ, health history, and how your body responds. But they don’t come without trade-offs. These drugs lower your body’s natural defenses, which means you’re more likely to catch infections, get sick from viruses others shake off, or even develop certain cancers over time. That’s why regular blood tests and doctor visits aren’t optional—they’re life-saving. You can’t just feel fine and assume everything’s okay. Blood levels need to stay in a narrow window. Too low? Rejection risk goes up. Too high? Toxicity kicks in. That’s why transplant medication management isn’t just about taking pills. It’s about tracking, testing, and talking to your care team every step of the way.
Many people don’t realize how much other meds can interfere. A simple over-the-counter painkiller, a herbal supplement like St. John’s wort, or even grapefruit juice can throw off your drug levels. That’s why your pharmacist needs to know every single thing you’re taking—prescription, OTC, or bought online. And it’s not just about drugs. Stress, poor sleep, or skipping meals can mess with how your body absorbs these medicines. You don’t need to live in a bubble, but you do need to be smart. Set alarms. Use pill organizers. Keep a written log. If you’re traveling, plan ahead—don’t wait until the last minute to refill. Most transplant centers have support teams just for this. Use them.
Below, you’ll find real-world guides on how to handle common drug interactions, spot early signs of trouble, and manage side effects without giving up your life. From comparing generic alternatives to understanding how liver health affects your meds, these posts give you the tools to stay in control—not just survive, but thrive after your transplant.