Ever start a new pill and within days feel weird-muscles sore, dizzy, or your face swells up? You might blame the drug right away. But what if the side effect doesn’t show up for weeks-or even months? Timing matters more than you think. The moment a side effect appears tells doctors a lot about what’s really going on. It’s not just about the drug. It’s about how your body reacts to it over time.
Some side effects hit fast. Others creep in slowly.
Not all side effects arrive the same way. Some hit like a lightning bolt. Others sneak up like a slow leak. This difference isn’t random. It’s built into the drug’s chemistry and how your body handles it.
Take antibiotics like ciprofloxacin. If you’re going to get nerve tingling or pain from it, it usually shows up in about 2 days. That’s one of the fastest known onset times for a common drug. Studies show women feel it even sooner than men-sometimes within 24 hours. This isn’t a coincidence. The drug builds up quickly in your system, and your nerves react fast.
On the other hand, ACE inhibitors like lisinopril can cause swelling in your face or throat-called angioedema-but not always right away. For some, it happens hours after the first dose. For others, it doesn’t show up until four months later. That’s not a mistake. It’s a known pattern. The body’s reaction changes over time, especially with drugs that affect the bradykinin system. If your doctor only checks for side effects in the first week, they might miss this entirely.
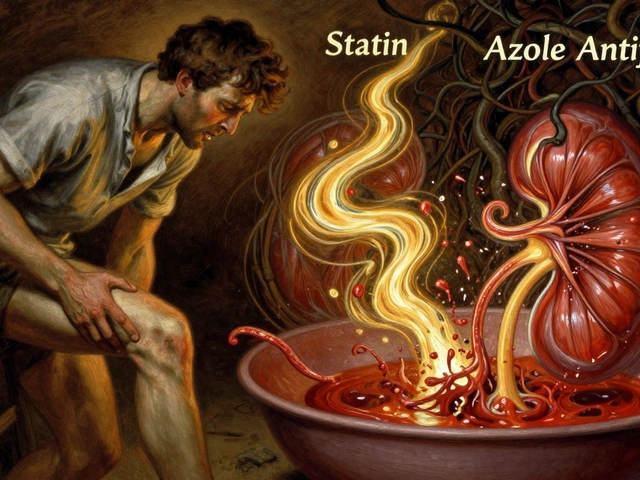
Statins don’t cause muscle pain the way you think they do.
Statins are the most prescribed drugs in the world. And muscle pain? That’s the #1 reason people quit them. But here’s the twist: research shows the pain often isn’t from the statin at all.
A major 2021 trial gave people either a statin or a sugar pill-and told everyone they were getting the real drug. People who thought they were on statins reported muscle pain. But so did people on the placebo. The pain started around the same time: 1 to 4 weeks after starting the pill. And when they stopped? Over half felt better in just 3 days, no matter which pill they took.
This isn’t about the drug. It’s about expectation. Your brain anticipates side effects. You feel a twinge in your leg, and suddenly it’s “the statin.” The drug might not be the cause. But the timing still matches up. That’s why doctors now ask: “When did the pain start? Before or after you started worrying about side effects?”
Antidepressants and anti-seizure drugs: the slow burn
Drugs like pregabalin and gabapentin are used for nerve pain and seizures. People often report dizziness or fatigue. Studies show most feel these effects within the first week. But the median time for them to show up? 19 days for pregabalin. That’s nearly three weeks. If you stop the drug at day 10 because you “feel awful,” you might be misreading the signal.
Same with interferon beta-1a, used for multiple sclerosis. Side effects like fatigue or flu-like symptoms can take over 500 days to appear. That’s more than a year. If a patient gets sick after 14 months, their doctor might never connect it to the drug. But the data says: yes, it’s possible. And it’s not rare.
These drugs don’t work like antibiotics. They change how your brain or nerves respond over time. The side effects build up slowly. That’s why you can’t judge them after a few days.
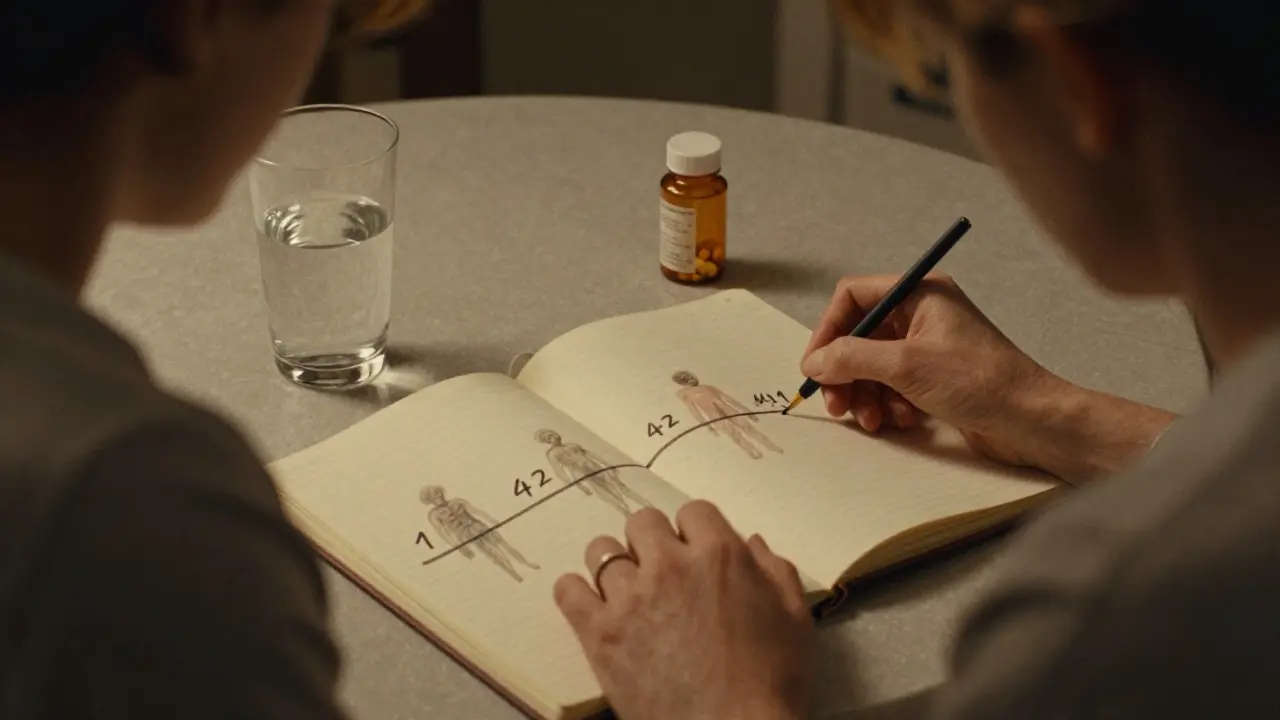
Drug-induced liver damage: the silent timer
Your liver processes almost everything you take. Sometimes, it reacts badly. The timing here is messy.
For most drugs, liver injury shows up around 42 days after starting. But that’s an average. It can be as early as 20 days-or as late as 117. That’s almost four months. If you’re on a new medication and start feeling tired, yellow-eyed, or nauseous after six weeks, don’t assume it’s the flu.
Then there’s acetaminophen (Tylenol). Take too much, and your liver fails-fast. Symptoms can show up in 24 hours. That’s not an idiosyncratic reaction. That’s direct toxicity. Different mechanism. Different clock.
Doctors use this timing to tell the difference: Is it a rare allergic reaction? Or an overdose? The clock tells the story.
Immune drugs: the delayed surprise
Drugs like natalizumab, used for multiple sclerosis, can cause nerve damage. But not right away. The median time? 141.5 days. That’s almost five months. Patients often feel fine for months. Then-suddenly-numbness, weakness, or trouble walking.
That’s a red flag. If your neurologist doesn’t know this pattern, they might think you’re getting worse from MS itself. But the timing doesn’t match MS progression. It matches the drug.
This is why post-marketing studies matter. A drug can pass clinical trials with flying colors-because side effects haven’t had time to show up yet. Real-world use reveals the hidden delays.
Why timing confuses doctors-and patients
Most people assume side effects happen fast. That’s what the pamphlet says. But real life doesn’t follow the brochure.
Patients often stop a drug too early-because they feel bad at day 5 and assume it’s the pill. But what if the real side effect hits at day 25? They miss it.
Or worse: they keep taking it for months, blaming every ache on “aging” or “stress,” while the drug quietly damages their liver or nerves. By the time they get tested, it’s too late.
Doctors, too, get fooled. If a side effect appears after 6 months, it’s easy to blame something else. But research shows: 37% fewer side effects are reported after a drug is stopped. Why? Because no one connects the dots anymore.
That’s why some hospitals now use software that flags side effects based on timing. If you started a new drug 12 weeks ago and now have unexplained fatigue? The system pops up a warning. It’s not perfect. But it helps.

What you can do: track your timeline
You don’t need to be a scientist to use this knowledge. Here’s how to protect yourself:
- Write down when you start each new medication. Keep it in your phone or a notebook.
- Note any new symptoms-and when they started. Even small stuff: a headache, a rash, trouble sleeping.
- Don’t assume it’s the drug right away. Wait. See if it gets worse, better, or stays the same over days or weeks.
- Bring your timeline to your doctor. Say: “I started this on [date]. I felt [symptom] on [date]. Is that normal?”
- Ask: “What’s the usual timing for side effects with this drug?” Most doctors won’t know. But if they do, they’ll appreciate you asking.
One patient on Drugs.com wrote: “I had angioedema 4 months after starting lisinopril. My doctor didn’t connect it until I showed him the research.” That’s power. You don’t need to be an expert. You just need to track time.
The future: personalized side effect clocks
Right now, we use averages. But the future is individual.
Scientists are starting to build models that predict your personal side effect timing based on your genes, age, sex, and even your gut bacteria. The NIH’s All of Us program is testing this now. In a few years, your doctor might say: “Based on your profile, you’re more likely to get nerve pain from this drug around day 18.”
Wearables are also getting involved. Companies are testing devices that track your movement, heart rate, and sleep patterns. If your activity drops suddenly 3 weeks after starting a new drug? The app might warn you: “Possible side effect detected.”
This isn’t sci-fi. It’s happening. And it’s going to change how we take medicine.
Bottom line: timing is part of the diagnosis
Side effects aren’t just about the drug. They’re about the clock. The same drug can cause different reactions at different times. Some hit fast. Some hit slow. Some hit when you least expect it.
Knowing when side effects typically appear doesn’t mean you’ll avoid them. But it means you won’t panic over a harmless twinge-or ignore a dangerous one.
Track your time. Ask questions. Don’t let assumptions hide the truth. Your body keeps a timeline. Learn to read it.


Comments(14)