When you're pregnant, even a simple headache or fever can feel like a crisis. You don’t want to take anything that might hurt your baby-but you also don’t want to suffer. So what’s safe? And when? The answer isn’t simple, but it’s clearer than you might think.
Acetaminophen: The Only Go-To Pain Reliever Through All Three Trimesters
Acetaminophen (also called paracetamol) is the only over-the-counter painkiller that doctors consistently recommend for use during every stage of pregnancy. From the first week of your first trimester to the final days before delivery, it’s considered safe when used as directed.
How much is safe? Standard doses: 325 to 1,000 mg every 4 to 6 hours. Don’t exceed 4,000 mg in a single day. Many people think they need to take the full 1,000 mg, but often 500 mg is enough. Use it for the shortest time possible-no more than 3 to 5 days in a row without talking to your provider.
Why is this important? Because untreated fever during pregnancy carries real risks. A 2017 study in Birth Defects Research found that a fever above 102°F in the first trimester can raise the chance of neural tube defects by up to 2.3 times. Pain and fever don’t just make you miserable-they can affect your baby’s development.
And what about the rumors? You’ve probably heard stories linking acetaminophen to autism or ADHD. A 2023 study in JAMA Network Open looked at nearly 100,000 mother-child pairs. The results? No meaningful connection. The adjusted odds ratio for autism was 1.03 (essentially no difference). For ADHD, it was 1.02. For intellectual disability, it was 0.98. In plain terms: if acetaminophen caused these issues, we’d see a clear spike in cases. We don’t.
Still, some experts have raised theoretical concerns about endocrine disruption. But even those researchers agree: the risk of not treating pain or fever is far greater. As Dr. Salena Zanotti from Cleveland Clinic says: "Acetaminophen is still the safest known drug to take during pregnancy for problems like fever and pain."
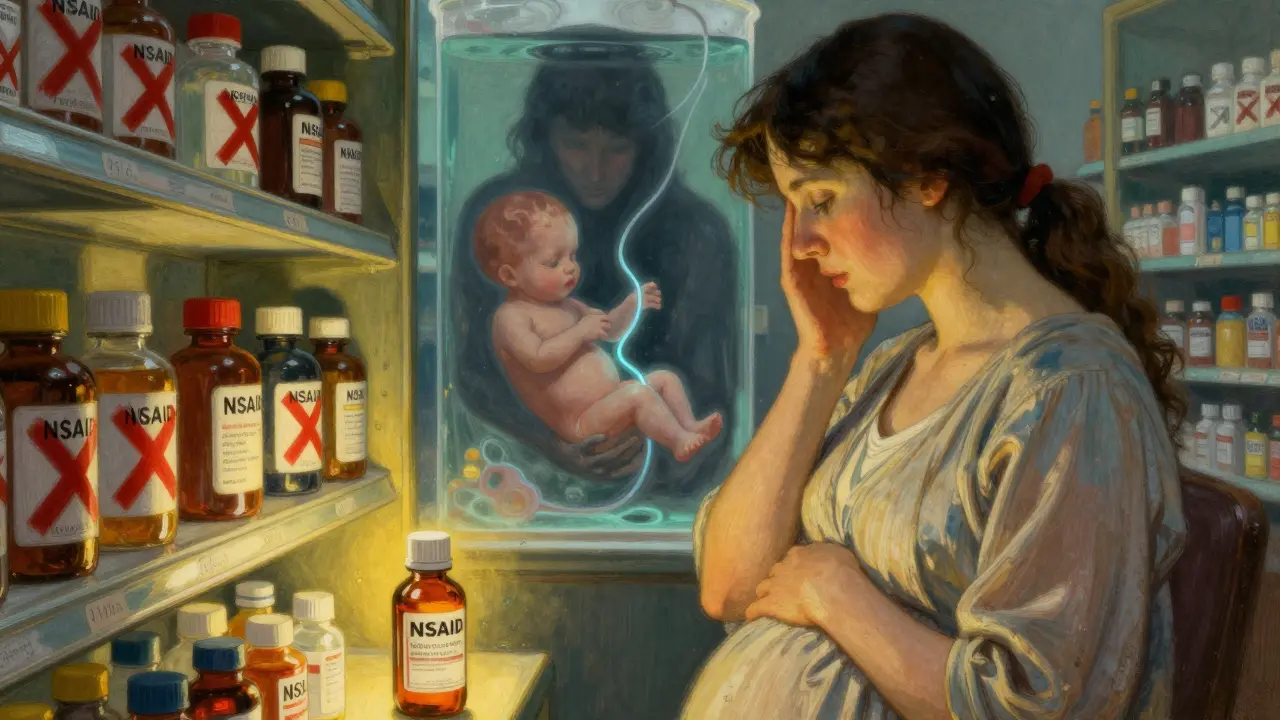
NSAIDs: A Hard Stop After 20 Weeks
NSAIDs-like ibuprofen (Advil, Motrin), naproxen (Aleve), and diclofenac (Voltaren)-were once thought to be okay before 30 weeks. That changed.
In October 2020, the FDA updated its warning: avoid NSAIDs at 20 weeks or later. Why? Because these drugs can shut down a key fetal blood vessel called the ductus arteriosus. This vessel helps blood flow properly in the developing baby. When it closes too early, it can cause serious heart problems.
Even more urgent: NSAIDs can trigger oligohydramnios-a dangerous drop in amniotic fluid. Within 48 to 72 hours of taking an NSAID after 20 weeks, a baby’s kidneys may start to struggle. Less fluid means less cushioning for the baby, and it can lead to lung underdevelopment, limb deformities, or even stillbirth.
Studies show that 1 to 2% of fetuses exposed to NSAIDs after 20 weeks develop oligohydramnios. Compare that to just 0.1% in unexposed pregnancies. That’s a 20-fold increase.
And here’s the tricky part: many cold and flu medicines contain NSAIDs. A 2023 FDA review found that 30% of OTC combination products list ibuprofen or naproxen as an ingredient-even if the main label says "pain reliever" without naming the drug. Always check the "Drug Facts" panel. If you see "ibuprofen," "naproxen," or "nonsteroidal anti-inflammatory," put it back.
What if you took one before you knew you were pregnant? Don’t panic. A single dose before 20 weeks carries very little risk. But if you’re past 20 weeks and you’ve been taking NSAIDs regularly, talk to your provider. An ultrasound to check amniotic fluid levels can give you peace of mind.
What About Aspirin?
Don’t confuse regular aspirin with low-dose aspirin. The FDA restriction doesn’t apply to 81 mg aspirin when it’s prescribed for preeclampsia prevention. This is a completely different use case. Low-dose aspirin is actively recommended for some high-risk pregnancies. But if you’re taking aspirin for headaches or muscle pain, it’s still an NSAID-and it’s not safe after 20 weeks.
Why Do So Many People Avoid Acetaminophen?
Here’s the real problem: misinformation. A 2023 survey by the American Academy of Family Physicians found that 68% of pregnant people avoid all pain medication. And 42% of them specifically avoid acetaminophen because of social media fear-mongering.
Reddit threads, TikTok videos, and blog posts paint acetaminophen as a silent danger. They cite correlation studies-like one that found more acetaminophen use in mothers of children with ADHD-and treat them like proof of cause. But correlation isn’t causation. Just because two things happen together doesn’t mean one caused the other. Maybe the mother was in pain because she had an infection. Maybe the infection, not the medicine, affected brain development. We don’t know. And we have better data now.
Dr. Magloire from the AAFP puts it bluntly: "I never recommend NSAIDs during any trimester because patients don’t always know how far along they are. Telling them it’s okay before 30 weeks-or even before 20 weeks-just creates confusion."
What Should You Do?
- For headaches, fever, or body aches: Use acetaminophen (500 mg) as needed. Stick to the lowest dose that works. Stop after 3-5 days if symptoms persist.
- For swelling, cramps, or inflammation: Don’t reach for ibuprofen. Talk to your provider. There may be non-drug options like heat packs, rest, or physical therapy.
- Check every OTC medicine: Read the Drug Facts label. If it says "ibuprofen," "naproxen," or "NSAID," skip it after 20 weeks. Even "multi-symptom" cold formulas can hide NSAIDs.
- Don’t assume "natural" is safer: Willow bark, ginger, or turmeric supplements aren’t regulated. Their safety in pregnancy isn’t proven. Stick to what’s been studied.
What’s Changing? What’s Next?
Guidelines keep evolving. In 2024, the NIH launched the Acetaminophen Birth Cohort Study, tracking 10,000 pregnancies to see if long-term use affects children’s brain development. Results won’t be ready until 2027.
Meanwhile, the FDA is reviewing whether acetaminophen labels need new warnings. Some researchers suggest genetic differences matter-15% of pregnant women have a gene variant (CYP2E1) that changes how their body breaks down acetaminophen. We don’t test for this routinely, but it’s a clue that future advice might get more personal.
For now, the message is clear: acetaminophen is the safest, most studied, and most effective option for pain and fever during pregnancy. The risks of not treating symptoms are far greater than the unproven risks of the medicine itself.
As Dr. Steven J. Fleischman, president of ACOG, said in September 2025: "The conditions people use acetaminophen to treat during pregnancy are far more dangerous than any theoretical risks."
Quick Summary
- Acetaminophen is safe in all trimesters when used at standard doses (325-1,000 mg per dose, max 4,000 mg/day).
- NSAIDs (ibuprofen, naproxen) are not safe after 20 weeks due to risk of fetal kidney damage and low amniotic fluid.
- Low-dose aspirin (81 mg) is safe if prescribed for preeclampsia prevention, but not for pain relief.
- Check OTC labels carefully-30% of cold/flu meds contain hidden NSAIDs.
- No credible evidence links acetaminophen to autism, ADHD, or intellectual disability in children.
Is acetaminophen safe during the first trimester?
Yes. Acetaminophen is the only over-the-counter pain reliever recommended for use in all trimesters, including the first. Untreated fever above 100.4°F during the first trimester can increase miscarriage risk by 1.5 times and raise the chance of neural tube defects. Acetaminophen is the safest way to bring down fever and manage pain during this critical time.
Can I take ibuprofen before 20 weeks?
Technically, yes-but it’s not recommended. While the FDA’s strict ban starts at 20 weeks, many providers avoid NSAIDs entirely during pregnancy because women often don’t know their exact gestational age. Even small doses before 20 weeks carry a small risk of early kidney effects. Acetaminophen is just as effective and has no known fetal risks. There’s no reason to risk it.
I took ibuprofen once at 22 weeks-should I be worried?
One dose is unlikely to cause harm. The biggest risk comes from repeated or prolonged use. If you took just one tablet, your provider may not even mention it. But if you’ve taken NSAIDs more than once or for more than a day after 20 weeks, ask for an ultrasound to check amniotic fluid levels. It’s a simple, non-invasive test that can give you peace of mind.
What if I have a migraine and acetaminophen doesn’t work?
Talk to your OB-GYN or midwife. There are pregnancy-safe prescription options for migraines, like certain anti-nausea drugs or triptans (in specific cases). Never self-medicate with NSAIDs. Your provider can help you find a solution that balances relief with safety.
Are there natural alternatives to acetaminophen?
Some people turn to ginger, turmeric, or acupuncture for pain relief. While these may help with mild discomfort, they don’t reliably reduce fever or treat moderate-to-severe pain. Acetaminophen is the only option proven to safely and effectively lower body temperature and relieve pain during pregnancy. Natural doesn’t always mean safer-especially when you’re dealing with something that could affect your baby’s development.