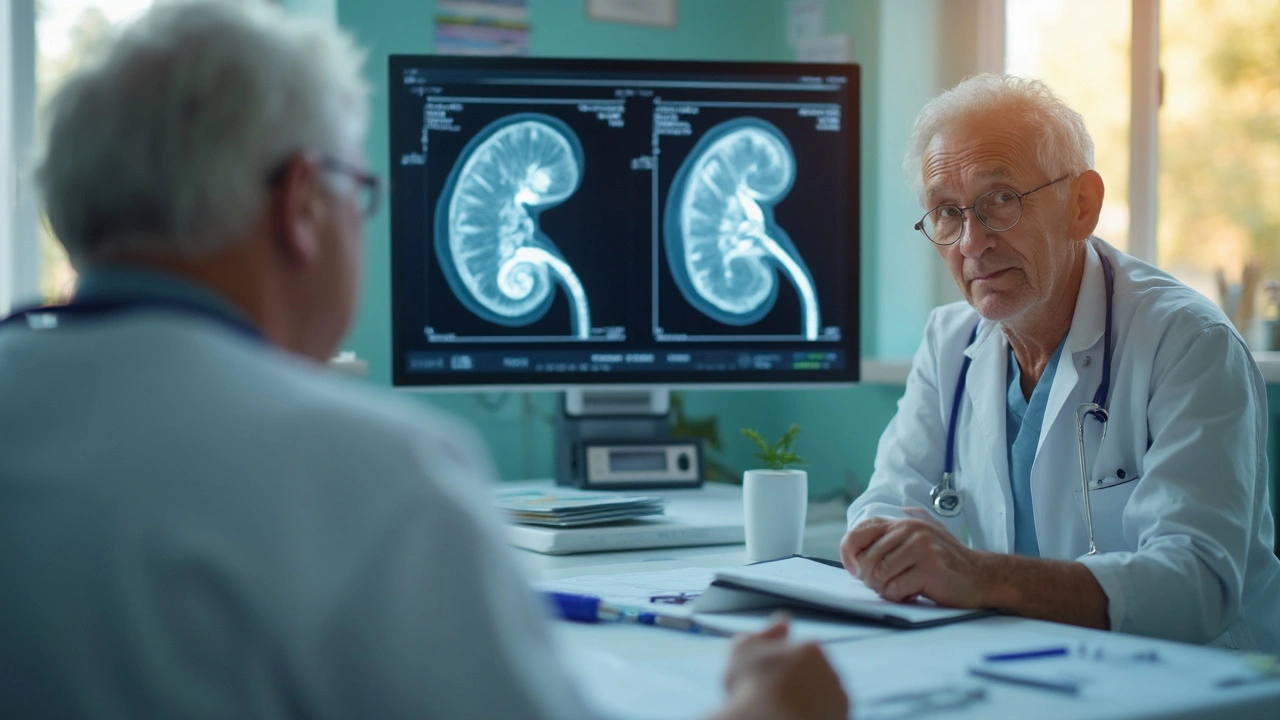
Picture this: ten years ago, most people with advanced renal cell carcinoma had only a handful of treatment choices, and none of them were easy. Surgery is tough—especially on older folks or those with other health issues—and chemotherapy barely makes a dent in this type of kidney cancer. But now, there's a surprising player on the scene: tumor ablation. Instead of open surgery, doctors can zap, freeze, or burn tumors right where they sit. It feels part science fiction, part medical magic—and it’s quickly moving from obscure to mainstream. So what’s the real story with ablation for kidney cancer? Let’s break down how it works, where it shines, and what you need to know if this is on your radar.
Understanding Renal Cell Carcinoma and Why Treatment Has Been So Challenging
Renal cell carcinoma isn’t your run-of-the-mill cancer. It starts in the tiny tubes of the kidney and, by the time it’s discovered, can already be playing hide-and-seek with the rest of the body. While early-stage RCC sometimes gets caught on routine scans, advanced cases often don’t cause symptoms until they’ve outgrown the kidney or popped up somewhere else—think lungs, bones, or even the brain. This sneaky nature means many are diagnosed when surgery alone isn’t an option. Standard treatments like targeted therapies (think sunitinib or pazopanib) and immunotherapies (like nivolumab) have made a difference, but they’re no walk in the park; side effects hit hard, responses can be hit-or-miss, and some tumors simply don’t play by the rules.
Historically, doctors leaned heavily on open or laparoscopic nephrectomy, yanking the whole kidney out if the tumor was confined. But kidneys aren’t spare parts, and not everyone handles major surgery well. Enter the idea of local tumor control: could you treat just the cancer in the kidney, with less collateral damage? That’s where ablation comes in—minimally invasive, quick recovery, and it leaves your plumbing mostly untouched. The appeal for advanced cases, especially for patients with cancer spread (metastasis) or with just one kidney left, is off the charts.
Let’s put some numbers on this. According to the American Cancer Society, about 81,800 people in the U.S. will be diagnosed with kidney cancer in 2024, and up to 30% of cases are already advanced when found. That’s a lot of folks needing something better than the blunt force of old-school treatments.
The Different Types of Ablation: Freezing, Burning, and Zapping Tumors
Okay, let’s talk tech. Ablation sounds fancy, but at its heart, it means destroying tissue with extreme temperatures or electric current. Doctors guide skinny needles right into the tumor—using real-time imaging like CT or ultrasound—then let the machine do the dirty work. Here’s a quick rundown of the main player techniques:
- Cryoablation: This one’s literally freezing the tumor, kind of like turning it into a cancerous popsicle. Liquid nitrogen or argon gas cools the probe down to -40°C, which crystallizes the tumor cells. Not surprisingly, they don’t survive the deep freeze.
- Radiofrequency Ablation (RFA): These probes use high-frequency electrical currents to generate heat. The temperature in the tumor can soar to 100°C—hot enough to cook the cancer cells from the inside out, but precise enough to spare nearby healthy parts.
- Microwave Ablation (MWA): Microwave energy produces even higher, more uniform heat than RFA. It’s a newer twist, being used more for larger or difficult-to-reach tumors, and it works fast—less than 10 minutes per session, in some cases.
- Irreversible Electroporation (IRE): This isn’t strictly about heat or cold—it uses high-voltage electrical pulses. The idea is to punch holes in the cancer cell membranes until the cells can’t function. It’s mainly used in research and for tumors close to delicate blood vessels.
Most ablation procedures are outpatient, meaning you’re in and out, and recovery is often just a few days. No massive incisions, no weeks in bed. A study published in European Urology in 2023 showed the average hospital stay for ablation was one day, versus four to eight days for surgery. My neighbor had RFA last year and walked Buddy with me the week after his session—no way would that have happened after a nephrectomy.

Who Benefits Most from Tumor Ablation? Patient Selection and Real Success Stories
Here’s the thing: ablation isn’t a slam dunk for everyone with kidney cancer. The best candidates are folks with small tumors (generally under 4 cm) or patients who can’t handle major surgery—either because of age, other illnesses, or already losing one kidney. But as techniques improve, doctors are pushing those boundaries. Right now, more than 25% of local treatments for early RCC worldwide are some form of ablation, and the number is climbing every year.
What about tough, advanced cases? This is where it gets interesting. Recent studies, including one in the Journal of Urology in late 2024 found that ablation could control symptoms, buy time, and sometimes shrink tumors even when the cancer had spread elsewhere. People with cancer in only certain spots (oligometastatic disease) seem to benefit most—knocking out a trouble-making mass while controlling other sites with drugs. Not only that, but ablation can be done repeatedly if new tumors pop up, so it’s a real tool for keeping cancer in check over time.
A patient I know, a 68-year-old dad who’d already lost a kidney, had cryoablation for a growing tumor last summer. He’s still working, spends weekends fishing, and left the hospital the next morning. His words: “I expected to feel broken, but I just felt relieved.” That’s the real magic—and the stories are piling up.
Of course, risks do exist. Kidney bleeding (hematoma), infection, or rare damage to nearby organs can happen. But rates for severe complications hover under 5%, far lower than major surgery. If the tumor is close to major vessels or the center of the kidney, ablation might not be safe or completely effective. That’s why imaging and careful planning are everything.
| Treatment Method | Average Length of Hospital Stay | Complication Rate | 5-Year Survival (localized)* |
|---|---|---|---|
| Ablation | 1 day | ~5% | 92% |
| Surgery (Partial/Full Nephrectomy) | 4–8 days | ~15% | 93% |
| Targeted Therapies | None (outpatient) | ~40% (moderate/severe side effects) | N/A |
*According to the SEER database (2024 US data) for localized RCC
The Future of Ablation: Integration with Drugs, Robotics, and What to Watch For
Ablation isn’t stopping here. The next wave is combining ablation techniques with the newer immune drugs—the idea being that killing the tumor with ablation actually wakes up the immune system, making immunotherapy drugs work even better. Early studies presented at ASCO 2024 hinted this could double survival times in some patients with advanced RCC. Researchers are also experimenting with guided robotic systems to make ablation even more accurate, especially for hard-to-reach tumors hiding deep in the kidney.
One little-known bonus: ablation can preserve kidney function much better than removing big chunks (or all) of your kidney. That means patients have a lower risk of ending up with chronic kidney disease, needing dialysis, or having to change their lifestyle completely. For folks like my uncle—who loves a greasy burger or a cold beer now and then—that’s a big deal.
If you're considering this route, here are a few real-world tips:
- Get a referral to an interventional radiologist or urologist who specializes in kidney ablation—not every hospital has the right gear or experience.
- Ask to see your scans and talk through exactly where the tumor sits. Location is everything for ablation success.
- Don’t skip the follow-up scans—recurrences are rare, but catching them early gives you more options if another ablation is needed.
- Bring a family member or buddy (your own or borrow mine, Buddy the Lab, he’s a great emotional support) to your appointments. It’s a lot to take in.
The bottom line? Ablation techniques are opening real doors for patients staring down advanced renal cell carcinoma. It’s less invasive, easier to bounce back from, and can offer a new kind of hope. As research heats up, expect to hear a lot more about these therapies—maybe even before Buddy gets his next treat.




Comments(6)