When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. But how do regulators know it’s truly the same? The answer lies in bioequivalence studies-rigorous, tightly controlled experiments that prove a generic drug delivers the same amount of active ingredient into your bloodstream at the same speed as the original. These aren’t theoretical guesses. They’re science-backed, regulatory-mandated tests that keep millions of people safe while saving billions in healthcare costs.
Why Bioequivalence Studies Exist
Before 1984, every generic drug needed its own full clinical trial to prove it worked. That meant long delays, higher prices, and fewer options for patients. The U.S. Hatch-Waxman Act changed that by creating a shortcut: if a generic drug behaves the same way in the body as the brand-name drug, it can be approved without repeating expensive human trials. This system now exists everywhere-from the FDA in the U.S. to the EMA in Europe and PMDA in Japan. The goal is simple: safe, effective, affordable medicine for everyone.The Core Idea: Same Drug, Same Effect
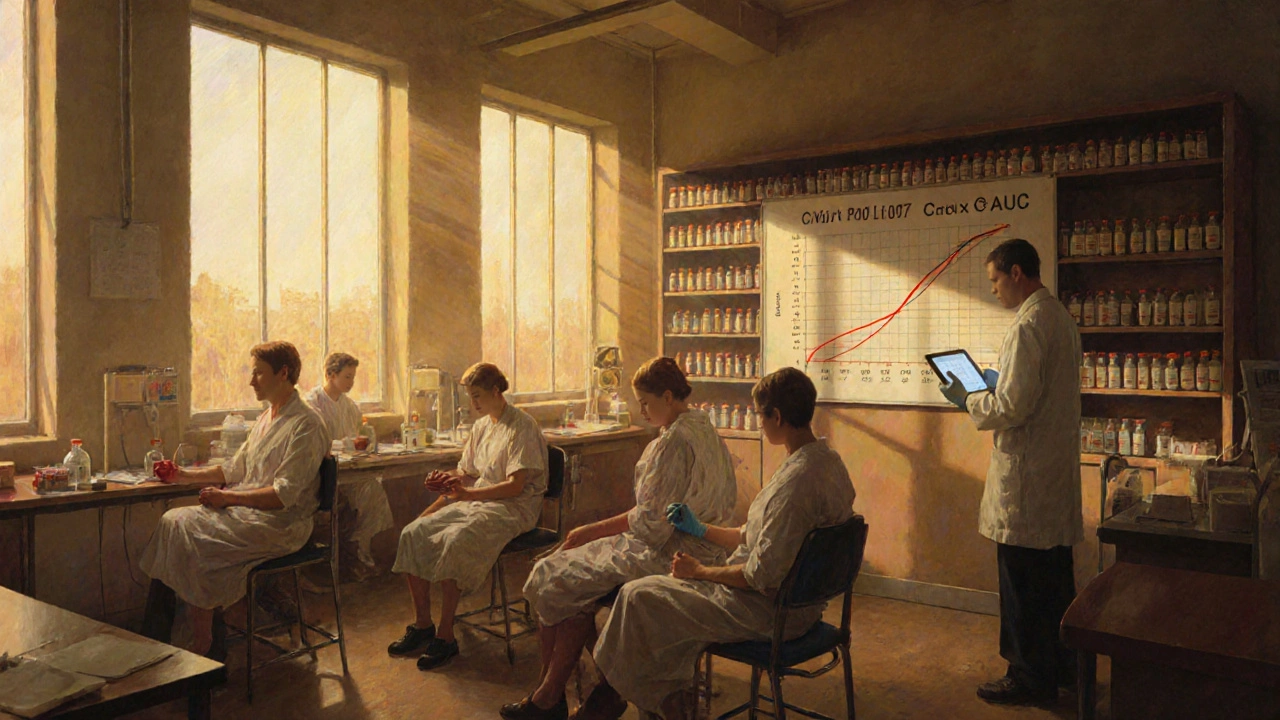
A bioequivalence study doesn’t test whether a drug cures a disease. It tests whether the body absorbs it the same way. Two key numbers matter: Cmax (the highest concentration of the drug in your blood) and AUC (the total amount of drug your body is exposed to over time). If the generic’s Cmax and AUC fall within 80% to 125% of the brand-name drug’s values, regulators consider them equivalent. For drugs with a narrow therapeutic index-like warfarin or lithium-that range tightens to 90% to 111%. This isn’t arbitrary. It’s based on decades of data showing that drugs within this range produce the same clinical results.Step 1: Choose the Right Reference Drug
Every study starts with one critical decision: which brand-name drug do you compare against? It’s not just any version. Regulators require the test product to be matched against a single batch of the original drug-called the Reference Listed Drug (RLD). This batch is chosen from three production lots, usually the one with a middle dissolution profile. Why? Because if the reference changes between studies, the results become meaningless. In practice, companies buy this batch directly from the brand manufacturer or through authorized distributors. Getting this wrong means your entire study is invalid.Step 2: Design the Study
The gold standard is a two-period, two-sequence crossover design. That means 24 to 32 healthy volunteers (sometimes up to 100 for tricky drugs) take both the generic and brand-name versions, but in random order. Half get the generic first, then the brand after a washout period. The other half get the brand first, then the generic. This design cancels out individual differences-like metabolism or body weight-because each person serves as their own control. The washout period? At least five half-lives of the drug. For a drug that clears in 12 hours, that’s 60 hours. For a slow-clearing drug like dutasteride (half-life of 5 weeks), it’s months. One CRO lost $250,000 and three months because they used a 14-day washout for a 72-hour half-life drug. The math didn’t add up. That’s why pilot studies are non-negotiable. They help you figure out the right washout time before you spend millions on the real thing.
Step 3: Collect Blood Samples
After each dose, blood is drawn repeatedly. Minimum? Seven time points: before the dose (time zero), one point just before peak concentration (Cmax), two around Cmax, and three during the elimination phase. Sampling continues until the area under the curve (AUC) captures at least 80% of the total exposure. For most drugs, that’s 3 to 5 half-lives. Blood is spun into plasma or serum, then analyzed using LC-MS/MS-a lab technique that can detect nanograms of drug per milliliter. The method must be validated to within ±15% accuracy (±20% at the lowest detectable level). If the lab’s assay is off, the whole study fails. BioAgilytix found 22% of studies get delayed because of analytical method issues-costing an average of $187,000 per delay.Step 4: Analyze the Data
Raw concentration numbers aren’t enough. They’re log-transformed because drug levels in blood follow a logarithmic pattern, not a straight line. Then, statisticians run an ANOVA model with fixed effects for sequence, period, treatment, and subject. The goal? Calculate the 90% confidence interval for the geometric mean ratio of test to reference for both Cmax and AUC. If both intervals fall between 80% and 125%, the drug is bioequivalent. If one value is outside-even by 0.1%-the study fails. No exceptions. That’s why biostatisticians need specialized training. One wrong assumption in the model can sink the entire submission.Step 5: Test Dissolution (For Some Drugs)
Even if the blood levels match, regulators still want to see how the drug dissolves in the lab. For most oral tablets, they test dissolution across pH levels from 1.2 (stomach) to 6.8 (intestine). At least 12 tablets per batch are tested at multiple time points. The similarity between the generic and brand-name dissolution profiles is measured using the f2 factor. If f2 is above 50, the profiles are considered similar. This step catches differences in formulation-like coatings or fillers-that might not show up in blood tests but could affect how the drug works in real life.
When the Standard Model Doesn’t Work
Not all drugs fit the two-period crossover model. For drugs with half-lives longer than two weeks, like some osteoporosis treatments, a parallel study is used-two separate groups, one gets the generic, the other the brand. For extended-release formulations, multiple-dose studies are required to see how the drug behaves over time. And for topical creams or inhalers, where the drug acts locally, pharmacodynamic or clinical endpoint studies are needed. For example, a generic asthma inhaler might be tested by measuring lung function, not blood levels. The FDA says you must use “the most accurate, sensitive, and reproducible approach available.” That’s why PK studies are used in 95% of cases-but not all.What Happens When It Fails
Failure rates are low-about 5% for simple generics-but they happen. Alembic Pharmaceuticals’ generic version of Trulicity was rejected in 2022 because Cmax values varied too much across studies. Why? The tablet’s coating didn’t dissolve consistently. The company had to reformulate, retest, and resubmit. That’s a $5 million setback. Common reasons for failure? Inadequate washout periods (45% of deficient studies), poor sampling schedules (30%), and statistical errors (25%). Pilot studies reduce failure rates from 35% to under 10%. Real-time analysis of blood samples during the study cuts protocol deviations by 40%. These aren’t just best practices-they’re survival tactics.Who Does This Work?
Bioequivalence studies are run by Contract Research Organizations (CROs) with teams of clinical operations staff, bioanalytical scientists, and biostatisticians. These aren’t entry-level jobs. Clinical staff need 6 to 12 months of BE-specific experience. Statisticians must master specialized ANOVA models. Lab technicians need years to perfect LC-MS/MS methods. The FDA receives about 2,500 bioequivalence submissions each year. The median review time? Just over 10 months. And with over 900 generic drugs approved in 2022 alone, this system is running at scale.What’s Next?
The field is evolving. The FDA is pushing for more use of modeling and simulation-especially for complex drugs like inhalers and biologics. BCS-based biowaivers (where dissolution data alone can replace a full study) now cover 27% of approvals. Japan’s PMDA still requires extra dissolution tests. The EMA and FDA still differ slightly on how to handle highly variable drugs. But the core remains unchanged: if the drug enters the bloodstream the same way, it works the same way. And for patients, that means more choices, lower prices, and no compromise on safety.What’s the difference between bioavailability and bioequivalence?
Bioavailability measures how much of a drug enters your bloodstream after you take it. Bioequivalence compares the bioavailability of two versions of the same drug-usually a generic and the brand-name version. One is a single measurement. The other is a comparison.
Why do bioequivalence studies use healthy volunteers instead of patients?
Healthy volunteers have no disease-related changes in metabolism, organ function, or drug interactions that could skew results. This gives regulators a clean baseline to see if the two drug versions behave the same way under normal conditions. Once bioequivalence is proven, the drug is approved for use in patients.
Can a generic drug be approved without a bioequivalence study?
Yes, but only in rare cases. For some BCS Class I drugs-those that are highly soluble and highly permeable-regulators may approve based on dissolution testing alone. This is called a biowaiver. It applies to less than 30% of generics. For most drugs, especially those with low solubility or complex formulations, a full pharmacokinetic study is required.
How long does a typical bioequivalence study take?
A single-period crossover study usually takes 3 to 6 weeks per subject, including screening, dosing, blood draws, and washout. The entire study-from planning to final report-can take 12 to 18 months. The regulatory review adds another 10 months on average. For complex drugs, timelines can stretch to two years.
Are bioequivalence studies safe for volunteers?
Yes. Volunteers are carefully screened for health conditions. Doses are kept low-often below therapeutic levels. Studies are monitored by independent ethics boards. Side effects are rare and usually mild-headache, nausea, or dizziness. Serious adverse events are extremely uncommon. Many volunteers participate multiple times, often for the compensation and the chance to contribute to medical science.





Comments(11)