Planning a trip when you’re living with postherpetic neuralgia travel tips can feel like juggling a suitcase full of medication, comfort gear, and endless what‑ifs. The good news? With the right prep, you can enjoy new sights without letting nerve pain steal the show.
Quick Takeaways
- Schedule a pre‑travel check‑up and update your pain‑management plan.
- Pack a travel‑ready medication kit: labeled containers, a copy of prescriptions, and a portable cooler if needed.
- Choose seats and accommodations that let you move freely and support affected areas.
- Bring non‑pharmacologic tools-compression garments, heat packs, TENS units-to complement meds.
- Secure travel insurance that covers chronic pain treatments and have a medical ID on you at all times.
What Is Postherpetic Neuralgia?
Postherpetic Neuralgia is a chronic neuropathic pain condition that persists after an outbreak of shingles (herpes zoster). The virus damages sensory nerves, leaving lingering burning, stabbing, or electric‑shock sensations that can last months or years.
About 10‑20% of adults over 60 develop PHN, and the pain often intensifies with temperature changes, stress, or prolonged immobility-factors you’ll encounter on a trip.
Why Travel Can Trigger PHN Flare‑Ups
Three main triggers tend to pop up on the road:
- Environmental shifts: Cold cabins, hot sun, or rapid altitude changes can aggravate nerve endings.
- Physical inactivity: Long flights or car rides limit circulation, increasing stiffness and pain.
- Stress: Unfamiliar schedules, jet lag, and planning hassles raise cortisol, which may amplify pain signals.
Understanding these triggers lets you craft a proactive strategy.
Pre‑Travel Medical Checklist
- Book a visit with your pain specialist 2‑4 weeks before departure. Review medication dosages, refill dates, and potential side‑effects on a new time zone.
- Ask for a written summary that includes drug names, strengths, and dosing intervals. Keep a digital copy on your phone.
- Confirm that any medication (e.g., gabapentin, duloxetine) you rely on is legal and not restricted in your destination country.
- Discuss non‑pharmacologic options-topical analgesics, TENS, or nerve blocks-and whether you can use them during travel.
- Arrange travel insurance that explicitly covers chronic pain care, emergency medication refills, and physiotherapy visits abroad.
- Order a medical ID bracelet or necklace that lists PHN, key meds, and emergency contacts.

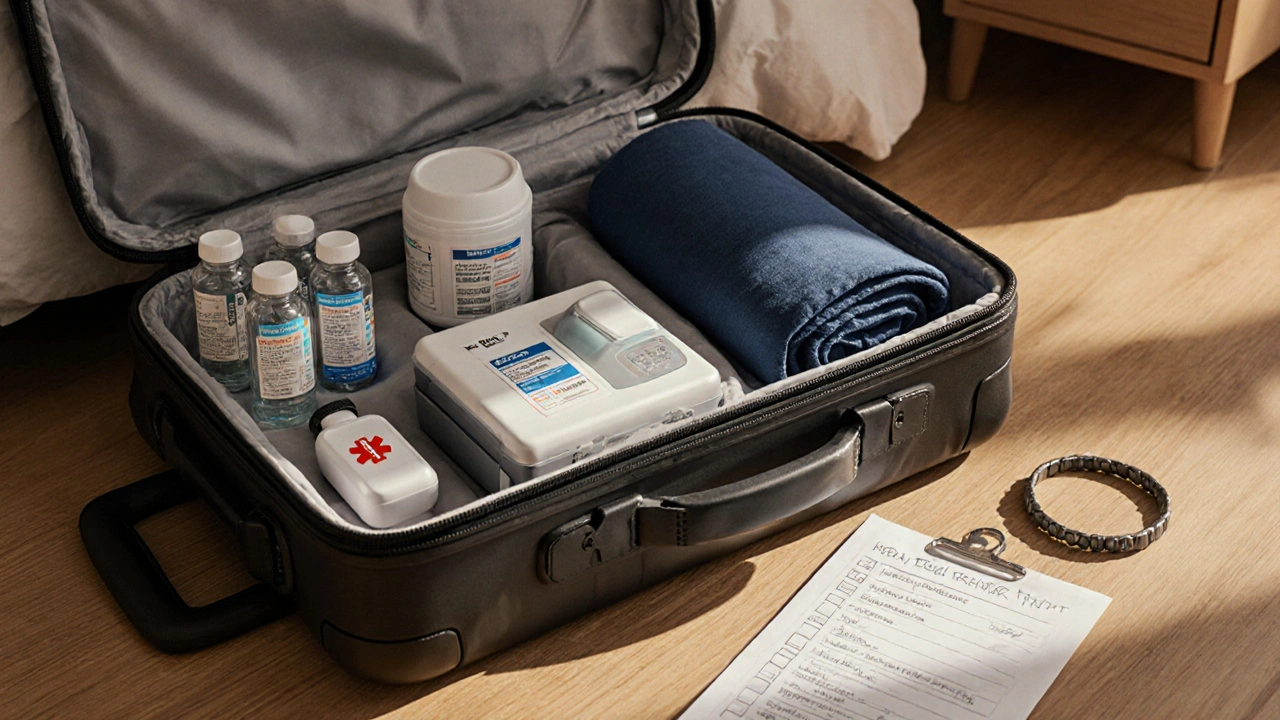
Pack Like a Pro: The PHN Travel Kit
Compartmentalize your kit into three sections: meds, comfort aids, and documentation.
| Category | Item | Why It Helps |
|---|---|---|
| Medication | Oral neuropathic agents (gabapentin, pregabalin) | Core pain control, maintain steady blood levels |
| Medication | Topical analgesic (lidocaine 5% patch) | Targeted relief without systemic side‑effects |
| Device | Portable TENS unit | Electrical stimulation reduces nerve firing |
| Gear | Compression garment or supportive sleeve | Improves circulation, eases muscle tension |
| Comfort | Heat pack (microwavable or chemical) | Soothes burning sensations during long layovers |
| Documentation | Prescription copies, doctor letter, insurance card | Smooth customs clearance, emergency care |
Label each container with the drug name, dosage, and “take with food” or “avoid alcohol” notes. A small cooler keeps heat‑sensitive meds stable on hot days.
Choosing Seats, Hotels, and Transport
- Airline seats: Opt for extra‑legroom or aisle seats so you can stretch every hour. Some carriers allow a “medical assist” request for a movable armrest.
- Ground transport: When possible, select seat‑back cushions that support the lower back and hips. A portable footrest can prevent pressure on the affected dermatome.
- Accommodation: Look for rooms with adjustable beds, easy bathroom access, and a mini‑fridge for meds. Hotels that provide a “quiet floor” reduce sensory overload.
Never sacrifice comfort for a lower price-pain‑induced stress can cost more in medical visits later.
Managing Pain During the Journey
Stick to a rhythm that mirrors your home schedule:
- Time‑zone alignment: Shift your medication times gradually a few days before departure. Use a phone alarm set to the destination’s local time.
- Stay hydrated: Dehydration heightens nerve sensitivity. Aim for 2‑3 liters of water per day, especially on flights.
- Move every 60‑90 minutes: Walk the aisle, stretch calves, and perform gentle shoulder rolls. Even a 5‑minute walk reduces stiffness.
- Temperature control: Dress in layers; carry a light blanket for cold cabins and a cooling scarf for hot climates.
- Stress reduction: Practice deep breathing or a short mindfulness app before boarding. A calm mind dampens pain signaling.
If pain spikes, apply a lidocaine patch or turn on your TENS unit for 15‑20 minutes. Document the episode in a travel pain diary to share with your doctor later.

Non‑Pharmacologic Comfort Tools
These accessories often make the biggest difference:
- Compression garment (e.g., thigh‑high sleeve): Provides gentle pressure, reducing nerve irritation.
- Heat pack: Warmth relaxes muscles around the affected skin area.
- Cold gel pack: Counteracts burning sensations during hot weather.
- TENS unit: Battery‑operated and approved for airline travel; use low‑frequency settings for neuropathic pain.
Test each tool at home before the trip to ensure you know how to apply it quickly.
Vaccination and Prevention for Future Trips
If you haven’t received the shingles vaccine, talk to your doctor about the recombinant zoster vaccine (RZV). Studies show a 90% reduction in PHN incidence for adults over 50. Getting vaccinated before traveling not only protects you but also lowers the chance of a new outbreak while abroad.
Health Safety and Insurance
Two safety nets are essential:
- Travel insurance: Verify coverage for chronic pain meds, physiotherapy, and emergency physician visits. Some policies require a pre‑approval form; keep it handy.
- Local medical facilities: Research hospitals or clinics near your itinerary that accept your insurance and have an English‑speaking staff.
Store emergency numbers in your phone and write them on a piece of paper in case the battery dies.
Frequently Asked Questions
Can I bring my prescription pain meds on a plane?
Yes. Keep them in original pharmacy bottles, label them clearly, and carry a doctor’s note. Place them in your carry‑on to avoid temperature extremes.
What if my pain worsens mid‑flight?
Use a lidocaine patch or TENS unit as soon as you notice a flare. Notify flight crew if you need extra blankets or a seat change for comfort.
Are there any foods that trigger PHN pain?
Highly processed foods and excessive caffeine can heighten nerve sensitivity. Opt for balanced meals with lean protein, whole grains, and plenty of fruits.
Do I need a special visa for medical treatment abroad?
Most tourist visas allow you to seek emergency care. For planned physiotherapy, check the destination’s health‑care regulations and your insurance policy.
How can I manage jet lag without worsening my PHN?
Gradually shift sleep times a few days before departure, stay hydrated, and use melatonin if needed. Avoid alcohol and heavy meals, which can trigger pain spikes.
Traveling with postherpetic neuralgia doesn’t have to be a nightmare. By checking your meds, packing smart comfort tools, and planning low‑stress logistics, you can turn a trip into a rewarding adventure instead of a pain‑filled ordeal.





Comments(10)