Most people know that high blood pressure can hurt your heart or kidneys. But few realize it’s quietly eating away at their vision-long before they notice any symptoms. Hypertensive retinopathy isn’t a flashy disease. It doesn’t come with sudden pain or blinding flashes. Instead, it sneaks in over years, silently damaging the tiny blood vessels in your retina. By the time you see blurred vision or dark spots, the damage may already be advanced. And here’s the kicker: you could have it right now and not know it.
What Exactly Is Hypertensive Retinopathy?
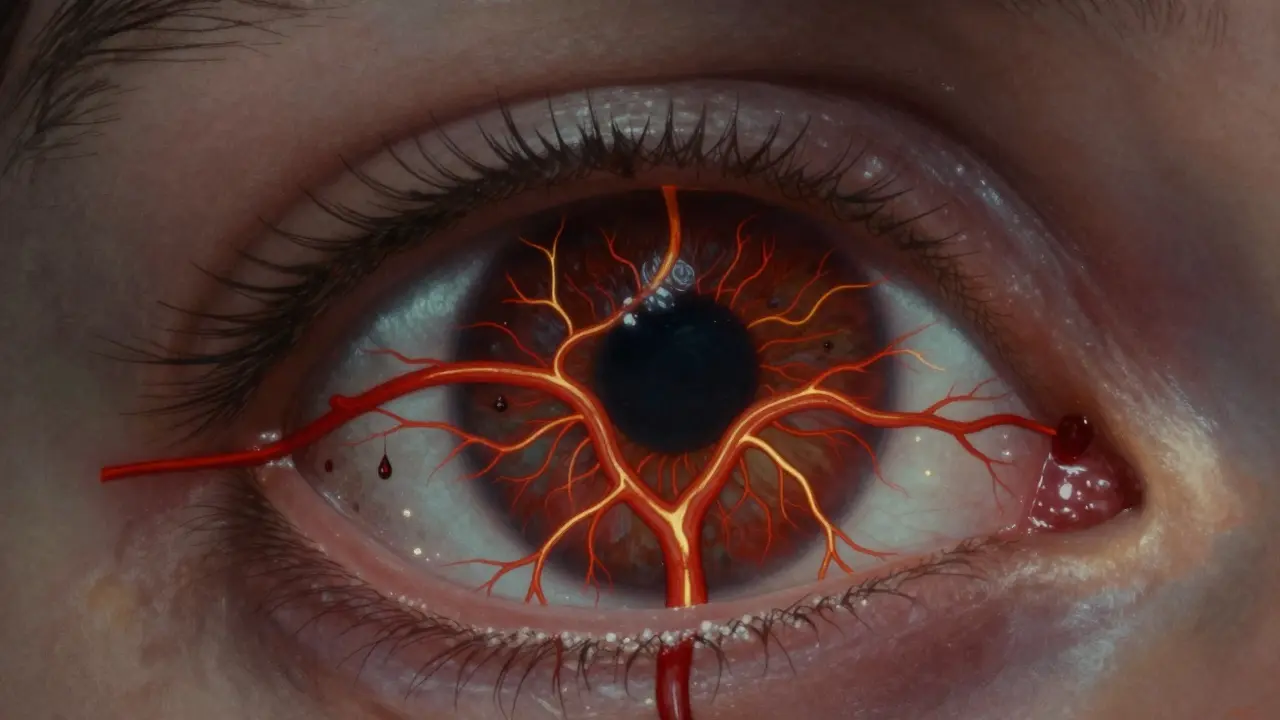
Hypertensive retinopathy happens when long-term high blood pressure forces your retinal blood vessels to thicken, narrow, and leak. The retina, the light-sensitive layer at the back of your eye, relies on a steady flow of oxygen-rich blood. When those vessels get squeezed or damaged, the retina starts to starve. Fluid, blood, and fatty deposits leak into the tissue, creating visible signs like hemorrhages, cotton wool spots, and hard exudates. These aren’t just eye problems-they’re warning signs your entire vascular system is under siege.
The Keith-Wagener-Barker system, developed in the 1930s and still used today, grades the damage into four stages:
- Grade 1: Mild narrowing of arteries. No bleeding or leaks yet.
- Grade 2: More narrowing, plus arteriovenous nicking-where arteries press down on veins like a thumb on a garden hose.
- Grade 3: Bleeding, fluid leakage, and cotton wool spots (tiny white patches from nerve damage).
- Grade 4: All of the above, plus swelling of the optic nerve (papilledema). This is a medical emergency.
Grade 4 isn’t just about vision-it means you’re at risk of stroke, heart attack, or kidney failure. Studies show patients with Grade 4 retinopathy have a 78% higher chance of having a stroke than those without it.
How High Does Blood Pressure Need to Be to Cause Damage?
You might think only severe hypertension causes eye damage. But that’s not true. The Merck Manual (2023) found that even "mild" hypertension-systolic pressure between 130 and 139 mmHg-can harm retinal vessels if left untreated for over 10 years. That’s not rare. According to CDC data from 2022, 13.9% of U.S. adults have stage 2 hypertension (140/90 or higher). Many more are in the "pre-hypertension" zone and don’t realize they’re already damaging their eyes.
Here’s what the numbers look like:
- After 3 years of uncontrolled BP ≥140/90, about 22% of people show early retinal changes.
- When systolic pressure hits 180 mmHg for six months or more, 35% develop retinal hemorrhages.
- Diastolic pressure over 120 mmHg triggers optic nerve swelling in 40% of cases within 72 hours.
And it’s not just about the number on the cuff. Duration matters just as much. Someone with 15 years of high blood pressure is far more likely to have advanced retinopathy than someone with 2 years-even if their numbers are the same.
Why You Might Not Notice It Until It’s Too Late
The scariest part? You can have Grade 1 or 2 retinopathy and feel absolutely fine. A 2023 ADA study found that 68% of people with early-stage damage report no vision problems at all. That’s why routine eye exams are non-negotiable if you have high blood pressure.
By the time symptoms show up, it’s often too late for full recovery. People with Grade 3 or 4 retinopathy commonly report:
- Blurred or dim vision
- Sudden dark spots or blind spots in central vision
- "Curtain-like" vision loss-like a shade pulling over part of your field of view
- Double vision with severe headaches (a red flag for malignant hypertension)
Reddit threads from r/Blindness and r/Hypertension are full of stories like this: "Woke up with a black spot in my right eye after my BP hit 210/110." Or: "I thought I had a migraine-turned out my retina was bleeding." Most of these patients didn’t connect their vision problems to their blood pressure until a doctor pointed it out.

How Doctors Spot It Before You Feel Anything
An eye doctor doesn’t need fancy machines to see early signs. A simple fundoscopic exam-where they shine a light into your eye and look at the back-can reveal narrowing arteries, nicking, or tiny hemorrhages. But technology is making detection faster and more accurate.
Optical coherence tomography (OCT) now shows changes in retinal thickness with micrometer precision. AI-powered tools like IDx-DR and the FDA-cleared RetinaCheck AI can analyze retinal images in seconds, spotting patterns humans might miss. A 2023 JAMA Ophthalmology study showed AI boosted diagnostic accuracy from 75% to 92%.
And it’s not just for specialists anymore. More primary care clinics are using handheld retinal cameras during routine checkups. If you have hypertension, ask your doctor: "Can you check my eyes for signs of retinopathy?"
Can the Damage Be Reversed?
Yes-but only if you act fast. The good news: the retina can heal if blood pressure drops quickly enough. Cleveland Clinic data shows that reducing systolic pressure by 25 mmHg within 48 hours resolves acute retinal changes in 65% of cases.
Here’s what recovery looks like:
- Within 7-10 days: Blurred vision often improves as fluid starts to reabsorb.
- Within 3-6 months: Macular swelling and exudates may shrink, improving central vision.
- Permanent damage? If the macula (the center of your vision) was scarred or if nerve fibers died, some vision loss is irreversible. About 22% of patients with advanced retinopathy end up with permanent visual field defects-even with perfect BP control.
That’s why early detection is everything. If you’re diagnosed with Grade 1 or 2, your vision can be preserved with consistent treatment. But wait until Grade 4? Your chances of saving your sight drop dramatically.

How to Protect Your Eyes If You Have High Blood Pressure
There’s no magic pill. No supplement. No eye drops. The only proven way to stop retinopathy is to control your blood pressure-and keep it under control.
Here’s what works:
- Take your meds as prescribed. Skipping doses-even once a week-lets pressure spike and damages vessels again.
- Monitor at home. Studies show 70% of people stick to their meds when they track their BP regularly. Get a validated upper-arm monitor. Take readings at the same time each day.
- Get your eyes checked yearly. If you have stage 2 hypertension or are over 50, do it every 6 months. The American Heart Association now recommends this for people with resistant hypertension.
- Watch your salt, sugar, and weight. A 10-pound weight loss can drop systolic pressure by 5-20 mmHg. Cutting sodium by 1,000 mg/day helps too.
- Choose the right meds. New research from the European Society of Cardiology shows ACE inhibitors reduce retinal damage progression by 32% compared to calcium channel blockers. Talk to your doctor about which drug is best for your eyes.
And don’t forget: if you’re diabetic, your risk of permanent vision loss jumps to 4.7 times higher when you also have high blood pressure. Managing both conditions isn’t optional-it’s life-saving.
What’s Next for Hypertensive Retinopathy?
The science is moving fast. The NIH launched the RETINA-HTN study in May 2023 to find genetic markers that predict who’s most vulnerable. Early results suggest 37 specific gene variants could identify high-risk patients before any damage shows up.
On the tech side, devices like RetiFlow-just completed Phase 3 trials-are making non-invasive blood flow measurements possible. No dye injections, no lasers. Just a quick scan that shows how well capillaries are perfusing the retina. Accuracy? 94% compared to the gold standard.
And insurance is catching up. Medicare now requires documentation of retinal exams for patients with stage 2+ hypertension under the 2023 Quality Payment Program. That means more people will get screened.
Final Thought: Your Eyes Are a Mirror
Hypertensive retinopathy isn’t just an eye disease. It’s a mirror. It shows you exactly what your blood vessels are doing everywhere else-in your brain, your heart, your kidneys. If your retina is damaged, your body is screaming for attention.
Don’t wait for blurry vision. Don’t assume you’re fine because you "feel okay." If you have high blood pressure, your eyes need to be checked-not just once, but every year. Because the damage doesn’t hurt until it’s too late. But the fix? It’s simple. Control your pressure. Stay consistent. And protect your sight before it’s gone.





Comments(9)