Generics make up over 90% of prescriptions filled in the U.S. They save patients and the system billions every year. But behind that number is a quiet, real risk: not all generics are created equal. Some work fine. Others? They can make patients sicker - not because they’re fake, but because of subtle differences in how the body absorbs them. Pharmacists are the last line of defense. And knowing when to flag a generic isn’t just good practice - it’s lifesaving.
What Makes a Generic Problematic?
A generic drug must have the same active ingredient, dose, and route as the brand-name version. The FDA says it’s bioequivalent if blood levels fall within 80-125% of the brand. Sounds tight? It’s not. That’s a 45% range. For most drugs, that’s fine. For others? It’s dangerous.
Take levothyroxine. A patient on a stable dose of 75 mcg for years. Switches to a new generic manufacturer. Six weeks later, their TSH jumps from 2.1 to 8.7. They’re tired, gaining weight, depressed. The doctor blames stress. The pharmacist? They notice the switch. They check the Orange Book. The new generic is still rated AB - legally equivalent. But the patient’s body didn’t get the same dose. That’s the gap between regulatory approval and real-world results.
It’s not just thyroid meds. Warfarin, phenytoin, digoxin, tacrolimus - these are narrow therapeutic index (NTI) drugs. The difference between a therapeutic dose and a toxic one is razor-thin. A 20% change in absorption can mean the difference between controlling seizures and causing them. The FDA has flagged 18 NTI drugs as high-risk. And studies show switching generics on these drugs increases failure rates by 2.3 times.
When to Flag: The Red Flags Pharmacists Can’t Ignore
Not every patient who says their generic ‘doesn’t work’ is wrong. Here’s when to dig deeper:
- Therapeutic failure within 2-4 weeks of a switch. If a patient’s blood pressure spikes, seizures return, or INR goes wild after a new generic is dispensed - don’t assume noncompliance. Check the manufacturer.
- Unexplained side effects after switching. Nausea, dizziness, rash - if these didn’t happen before but started after a new generic, document it. The FDA’s MedWatch database shows 28.1% of patient complaints about generics involve unexpected side effects after manufacturer changes.
- Multiple switches in a short time. A patient on levothyroxine who’s been switched three times in six months? That’s a recipe for instability. Even if each switch is technically ‘equivalent,’ the cumulative effect matters.
- Complex formulations. Extended-release pills, inhalers, topical creams, injectables - these are harder to copy. In 2020, FDA testing found 7.2% of generic extended-release opioids failed dissolution tests. That’s not a typo. Seven percent of these pills didn’t release the drug as designed.
- Look-alike, sound-alike names. Oxycodone/acetaminophen vs. hydrocodone/acetaminophen. The labels look similar. The bottles look similar. A quick mix-up can lead to overdose. ASHP reports 14.3% of generic errors come from this. Always double-check the manufacturer and strength.
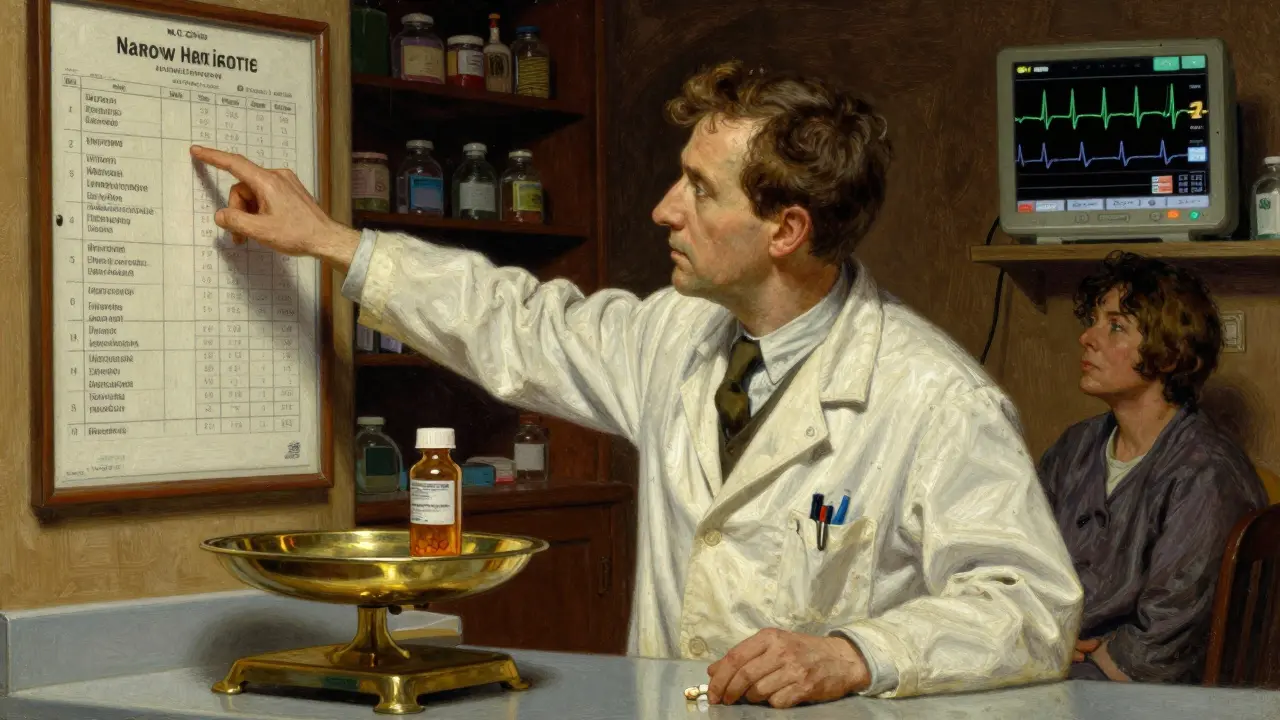
The Orange Book Isn’t Enough - But It’s Your Starting Point
The FDA’s Orange Book lists therapeutic equivalence codes. AB means ‘therapeutically equivalent.’ BX means ‘not equivalent.’ But here’s the catch: many generics are still rated AB even if they’ve had issues. Why? Because the rating is based on one bioequivalence study - not real-world outcomes.
Pharmacists need to go beyond the code. Look at the manufacturer. If a patient had a problem with a generic from Company X last month, and the same drug from Company X shows up again? Flag it. Document the manufacturer every time. A 2022 University of Florida study found that 68.4% of therapeutic failure investigations required knowing the specific manufacturer. Without that, you’re flying blind.
Who’s Most at Risk?
It’s not just elderly patients on multiple meds. It’s anyone on a critical drug:
- Patients with epilepsy - one missed dose can trigger a seizure.
- Heart transplant recipients on tacrolimus - a small drop in blood levels can mean organ rejection.
- Patients on warfarin - a slight change in INR can cause a stroke or internal bleeding.
- People with chronic kidney disease - their bodies process drugs differently.
- Children and pregnant women - their metabolism isn’t the same as adults.
And here’s something many don’t talk about: patients who’ve been stable for years. They’re the ones who get switched without warning. A pharmacy system auto-substitutes. The patient doesn’t notice. Until they feel awful.

What You Can Do - Right Now
You don’t need a PhD to protect patients. Here’s what works:
- Always note the manufacturer on the label. Use your pharmacy system’s notes field. Write it down. Even if it’s not required, it’s your paper trail.
- Ask patients: ‘Have you noticed any changes since your last refill?’ Don’t wait for them to complain. Ask. Especially if it’s an NTI drug.
- Don’t automatically substitute for NTI drugs unless the prescriber says ‘dispense as written.’ In 4 states - Massachusetts, New York, Texas, and Virginia - pharmacists are legally required to get explicit permission before switching NTI generics. Even if you’re not in one of those states, treat it like a rule.
- Report bad batches. Use the FDA’s MedWatcher app. It takes 4.7 minutes. One report might save a life. The ISMP reported a 18.3% increase in pharmacist-reported incidents after mandatory reporting started in 15 states. Your voice matters.
- Stay updated on recalls and alerts. The FDA issued a warning in 2023 about inconsistent dissolution in generic diltiazem CD. That led to 47 cases of therapeutic failure. If you’re dispensing diltiazem, know which manufacturer has the issue.
It’s Not About Trusting or Distrusting Generics
Most generics are safe. Most are excellent. But the system isn’t perfect. The FDA inspects over 2,000 facilities a year. In 2022, they found 187 data integrity issues and 243 quality control failures. That’s not a few bad apples. That’s a systemic risk.
Pharmacists aren’t here to fight the system. We’re here to protect patients from its gaps. The cost savings of generics are real. But they shouldn’t come at the cost of safety. When a patient says, ‘This doesn’t feel right,’ listen. When a TSH climbs after a switch, investigate. When a drug from a new manufacturer causes side effects - don’t shrug. Document. Report. Flag it.
Because in pharmacy, it’s not just about filling prescriptions. It’s about knowing when the script might be wrong - even if the label says it’s right.
Are all generic drugs safe?
Most are. Over 90% of prescriptions in the U.S. are filled with generics, and the vast majority work just as well as brand-name drugs. But safety isn’t guaranteed. Some generics, especially for narrow therapeutic index drugs like levothyroxine or warfarin, can cause problems due to small differences in how they’re absorbed. Regulatory standards allow for up to a 20% variation in drug exposure - enough to matter in sensitive cases.
What are narrow therapeutic index (NTI) drugs?
NTI drugs have a very small window between a therapeutic dose and a toxic one. Examples include levothyroxine, warfarin, phenytoin, digoxin, and tacrolimus. Even a small change in blood levels can lead to treatment failure or serious side effects. Switching between generic manufacturers of these drugs increases the risk of adverse events by more than twice compared to non-NTI drugs.
Can a generic drug be legally equivalent but still cause problems?
Yes. The FDA rates generics as ‘AB’ (therapeutically equivalent) based on bioequivalence studies, but those studies don’t always reflect real-world outcomes. A 2023 FDA alert identified generic diltiazem CD products with inconsistent dissolution profiles - meaning the drug didn’t release properly - leading to 47 cases of therapeutic failure. The product was still rated AB, but patients suffered.
Why do some patients say their generic doesn’t work?
Patients often report changes in effectiveness or side effects after switching manufacturers. This can happen with complex formulations like extended-release pills, where the drug’s release mechanism differs slightly between brands. Gastrointestinal drugs, thyroid meds, and seizure medications are common culprits. In one survey, 41.5% of pharmacists reported patient complaints about generic efficacy - especially with delayed-release products.
What should I do if I suspect a problematic generic?
First, document the manufacturer, lot number, and patient symptoms. Check the FDA’s Orange Book for the therapeutic equivalence rating. If it’s an NTI drug, contact the prescriber and suggest switching back to the previous version or using the brand. Report the issue to the FDA’s MedWatch program or the Institute for Safe Medication Practices. One report can trigger a broader investigation.






Comments(14)