When you order your generic medication through the mail, you’re not just getting a cheaper pill-you’re getting a product that has passed through a highly controlled system designed to protect its quality from factory to your doorstep. Many people assume that because generics are cheaper, they’re somehow less reliable. But that’s not true. In fact, the systems behind mail-order pharmacies are often more rigorous than those in your local pharmacy. Here’s what actually happens between the time a generic drug leaves the manufacturer and lands in your medicine cabinet.
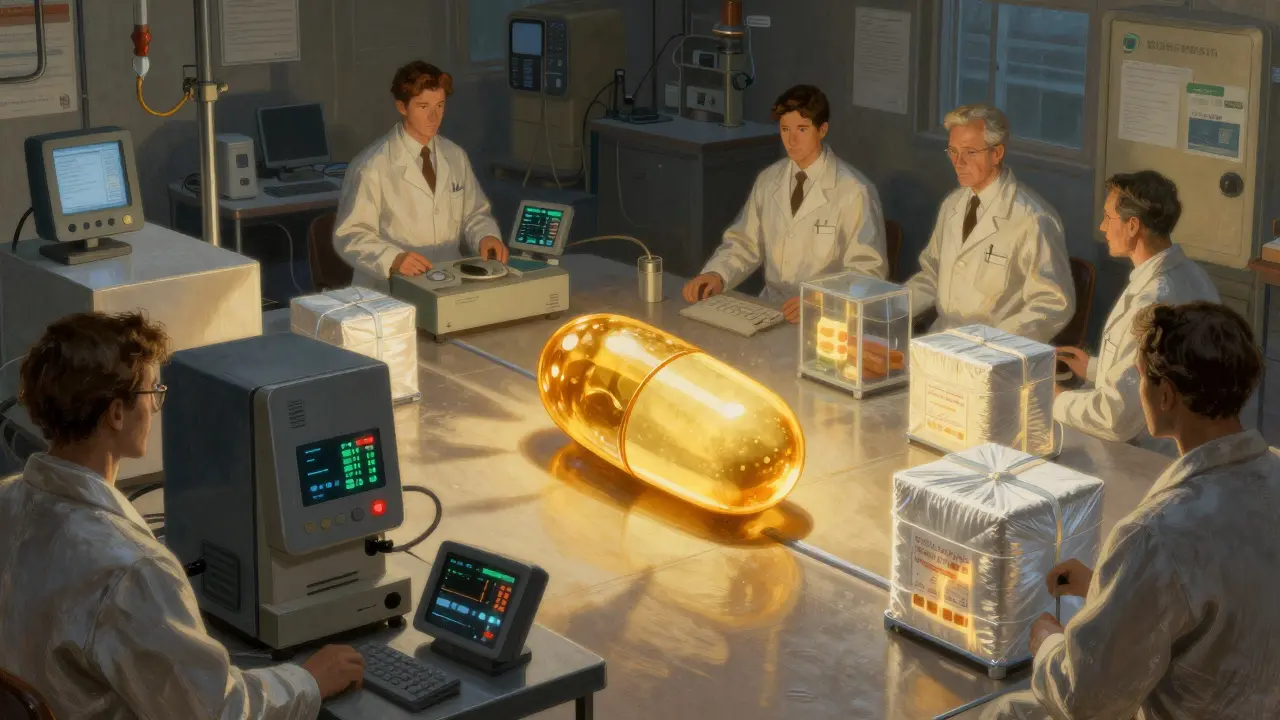
How Generic Drugs Are Made and Verified
Every generic drug you receive through mail-order must meet the same standards as its brand-name version. The FDA requires that generics have the same active ingredient, strength, dosage form, and route of administration. But it doesn’t stop there. The agency also demands that the generic drug performs the same way in your body. This means the amount of medicine your bloodstream absorbs-called bioavailability-must be within 80% to 125% of the brand-name drug. In practice, most generics fall within just 4% of the original, according to the FDA’s own bioequivalence database.
Manufacturers don’t get a pass just because they’re making a generic. They must follow Current Good Manufacturing Practices (cGMP), which are strict rules outlined in 21 CFR Parts 210 and 211. These cover everything from how raw materials are stored to how finished pills are packaged. Every batch of generic medication is tested using high-performance liquid chromatography (HPLC), a method that can detect differences as small as 0.1%. If a batch doesn’t match the reference drug exactly, it’s rejected. No exceptions.
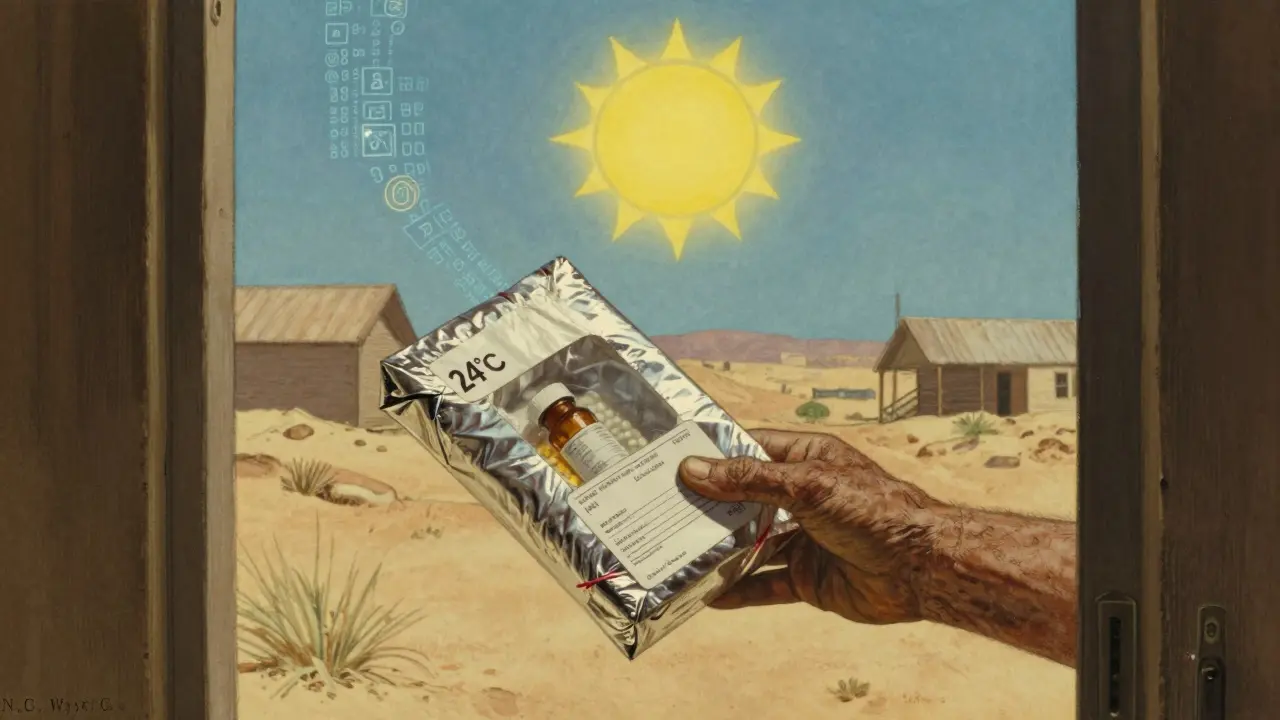
Temperature Control: The Hidden Battle for Stability
One of the biggest challenges in mail-order pharmacy isn’t the drug itself-it’s keeping it stable during transit. Many generics, like levothyroxine or insulin, are sensitive to heat, cold, or moisture. A pill that’s fine in a cool, dry pharmacy shelf might degrade if it sits in a hot truck for three days.
Mail-order pharmacies don’t use cardboard boxes and bubble wrap like your Amazon orders. They use insulated shipping containers with phase-change materials that act like thermal batteries. These can keep medications within safe temperature ranges-usually 20-25°C for most drugs, or 2-8°C for refrigerated ones-for up to 10 days. That’s far longer than the 2-4 hours a standard retail take-home bag can protect.
Every storage facility has continuous temperature monitors that log data every 15 minutes. That’s 96 readings per day per room. If a unit spikes above 27°C for more than 15 minutes, the system alerts staff immediately. Some facilities even use predictive analytics: if the forecast says it’ll hit 95°F in Phoenix next week, they automatically upgrade packaging for all shipments going there. CVS Caremark’s 2022 initiative cut temperature excursions by 63% using this method.
Tracking Every Pill: Serialization and Barcodes
Each generic medication you receive has a unique serial number tied to its National Drug Code (NDC). This isn’t just for inventory-it’s a legal requirement under the Drug Supply Chain Security Act (DSCSA), which went fully into effect in November 2023. Every time a pill moves-whether from the warehouse to the packing line to the delivery truck-it’s scanned and logged. This creates a digital trail that can trace a single pill back to the manufacturer, even if it’s shipped across the country.
Mail-order pharmacies use barcode scanning at least four times during fulfillment: when the drugs arrive, when they’re picked for your order, when they’re packed, and when they leave the facility. This system achieves 99.98% order accuracy, according to Express Scripts. That means fewer wrong pills, fewer missed refills, and fewer calls to customer service.

Why Mail-Order Has Fewer Errors Than Retail
You might think a local pharmacy with face-to-face interaction would be more careful. But the opposite is often true. Retail pharmacies handle hundreds of prescriptions a day, often under time pressure. Mail-order pharmacies operate like precision factories. They fill thousands of the same prescription at once. That means pharmacists can focus on consistency rather than speed.
For high-risk generics-like warfarin or insulin-mail-order pharmacies require double verification. Two pharmacists check the label, the dose, and the patient’s profile before it leaves the building. Retail pharmacies rarely do this. URAC, the accreditation body for mail-order pharmacies, requires 30% more quality checkpoints than standard retail practice. That includes mandatory annual training for pharmacists on generic drug equivalence. Most accredited facilities require 15 hours of continuing education each year.
What Happens When Things Go Wrong
Even with all these safeguards, problems happen. The biggest issue? Temperature excursions during extreme weather. Reddit users report duloxetine capsules becoming sticky after sitting in a hot mailbox for days. Trustpilot reviews show 23% of negative feedback mentions insulin or other biologics arriving warm. These aren’t isolated cases. In 2023, the FDA issued three warning letters to mail-order pharmacies for failing to maintain temperature controls during summer months.
Another problem: returns. Once a medication leaves the pharmacy, FDA rules forbid it from being restocked-even if it’s unopened. That means if you don’t pick up your package or decide not to take the drug, it gets thrown away. Mail-order pharmacies report about 7% waste, compared to 2-3% at retail. That’s a financial and environmental cost that’s rarely discussed.
Who’s in Charge? The Big Players and Their Standards
Three companies-Express Scripts, OptumRx, and CVS Caremark-handle 78% of all mail-order generic prescriptions in the U.S. They don’t just compete on price; they compete on quality. Each has invested millions in temperature-controlled warehouses, real-time tracking systems, and pharmacist training programs. Express Scripts alone spends over $2 million annually on serialization compliance alone.
Independent mail-order pharmacies make up the remaining 22%. They often partner with larger distributors to access the same quality systems. But they’re held to the same standards. Whether you’re getting your metformin from a Fortune 500 company or a small regional pharmacy, the FDA rules are identical.
What Patients Are Saying
Consumer Reports surveyed 2,345 mail-order users in 2023. 87% said their generic medications felt just as effective as brand-name versions. One user wrote: “I’ve been on the same Teva generic metformin for five years. Same imprint, same color, same size. Never had an issue.”
But trust isn’t blind. 34% of respondents admitted they worried about shipping conditions. And that’s fair. The FDA doesn’t require real-time GPS and temperature tracking yet-but it’s coming. Their 2024-2028 strategic plan includes pilot programs for smart packaging that sends alerts if a shipment overheats. Some companies are already testing blockchain systems to verify drug authenticity. Express Scripts’ pilot cut counterfeit incidents by 40%.
Is It Safe? The Bottom Line
Yes, mail-order generic medications are safe. The FDA oversees them just as closely as brand-name drugs. The systems in place-temperature control, serialization, double-checking, and strict testing-are more advanced than what most retail pharmacies use. The idea that generics are “inferior” because they’re cheaper is outdated. They’re not just equivalent-they’re often more consistently made.
That said, if you’re taking a narrow therapeutic index drug-like levothyroxine, warfarin, or cyclosporine-pay attention to how your body responds. Some research suggests even small variations can affect outcomes in sensitive patients. If you notice a change in how you feel after switching to a new generic, talk to your pharmacist. Don’t assume it’s all in your head.
And if you live in a hot climate? Ask your mail-order pharmacy what kind of packaging they use. Ask if they adjust for weather. You have a right to know.
Are mail-order generic drugs as effective as brand-name drugs?
Yes. The FDA requires that generic drugs have the same active ingredient, strength, and dosage form as the brand-name version. They must also deliver the same amount of medicine into your bloodstream within a very tight range-typically within 4% of the original. This is verified through rigorous testing using HPLC and bioequivalence studies. Thousands of patients use generics daily without any loss in effectiveness.
Can temperature changes during shipping ruin my generic medication?
It’s possible, but unlikely with reputable mail-order pharmacies. They use insulated packaging with phase-change materials that maintain safe temperatures for up to 10 days. Facilities monitor temperature every 15 minutes and upgrade packaging based on weather forecasts. Still, if you live in a very hot area and your medication arrives warm or sticky, contact your pharmacy. They should replace it at no cost.
Why do my generic pills look different each time I refill?
Different manufacturers make the same generic drug. The FDA allows multiple companies to produce a generic, and each uses different inactive ingredients (like dyes or binders), which can change the pill’s color, shape, or size. But the active ingredient and dosage remain identical. This doesn’t affect effectiveness-it’s just a result of how generics are produced. If you’re concerned, ask your pharmacist to stick with one manufacturer.
Do mail-order pharmacies test every batch of generic drugs?
Yes. Every incoming batch of generic medication is tested for identity, strength, purity, and quality against the brand-name reference drug. This is done using validated HPLC methods that detect variations as small as 0.1%. These tests are required by the FDA and are part of the cGMP standards that mail-order pharmacies must follow.
What happens if my medication is damaged or lost in the mail?
Mail-order pharmacies are required to replace damaged or lost medications at no cost. Because they track every package with barcodes and serial numbers, they can quickly verify delivery issues. If your pills arrive wet, melted, or missing, call their pharmacy hotline-most respond within 47 seconds. You’re not responsible for the cost of replacement.
Are mail-order pharmacies regulated differently than retail pharmacies?
They follow the same FDA rules, but mail-order pharmacies are held to stricter operational standards. URAC accreditation, which most major providers hold, requires 30% more quality checks than retail pharmacies. This includes double verification for high-alert drugs, continuous temperature logging, and 15 hours of annual training for pharmacists on generic drug standards. The goal is consistency at scale.





Comments(12)