Medication Splitting Safety Checker
Is Your Medication Safe to Split?
Check if your medication can be safely split to reduce side effects. Only medications with a wide therapeutic index and immediate-release formulations are typically safe to split.
Enter a medication name to see if it's safe to split
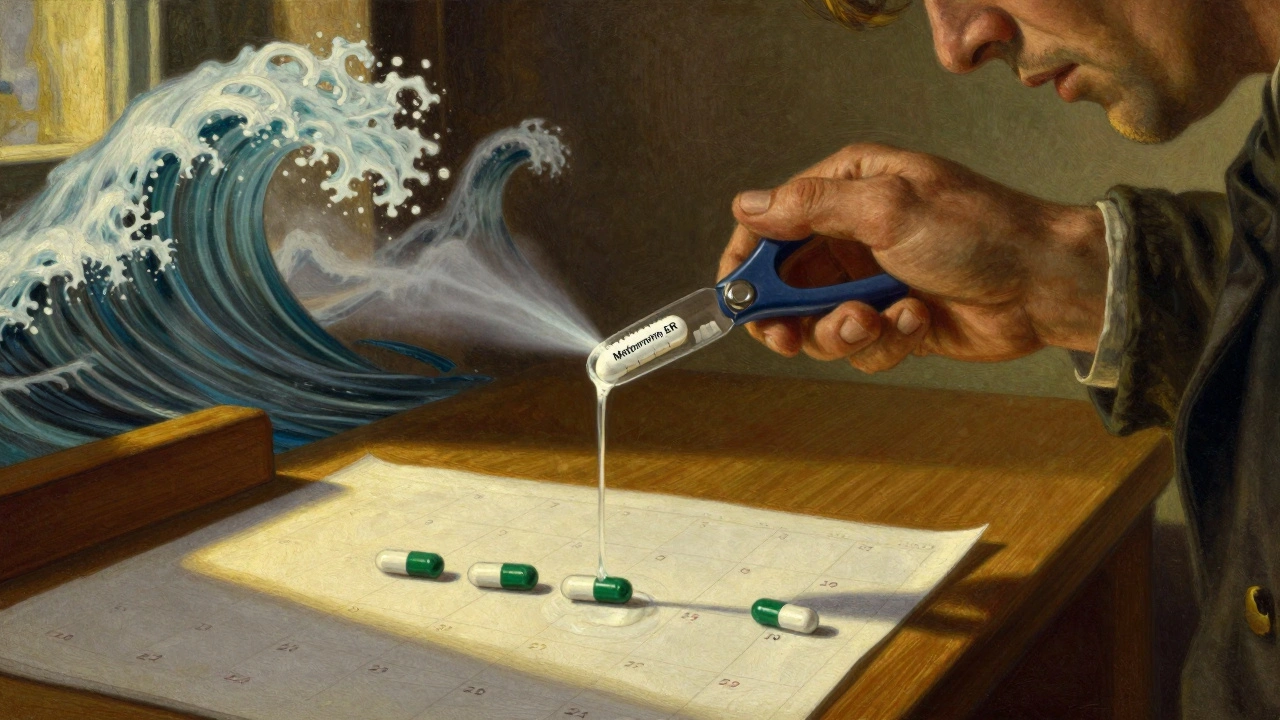
Ever taken a pill and felt awful an hour later-nausea, dizziness, a pounding headache-only for it to fade by lunchtime? You’re not imagining it. That spike in how you feel isn’t just bad luck. It’s your body reacting to a peak in drug concentration. And sometimes, splitting your daily dose into smaller, more frequent doses can smooth out those spikes and make side effects much easier to handle. But here’s the catch: not all pills can be split. Some will make things worse. A lot worse.
What Actually Happens When You Take a Pill?
When you swallow a tablet, your body doesn’t just slowly absorb it like a sponge soaking up water. It’s more like pouring a cup of coffee into a narrow glass. The drug hits your bloodstream fast, climbs to a high point (the peak), then slowly drops. For some drugs, that peak is the problem. High peaks mean more side effects. Lower, steadier levels mean better tolerance. Take metformin, for example. A lot of people with type 2 diabetes get stomach cramps, diarrhea, or nausea when they take 1000mg twice a day. But if they split that same 2000mg total into 500mg four times a day? Many report those side effects drop by more than half. Why? Because their blood never hits that high, jarring peak. The same principle applies to immediate-release opioids like oxycodone-splitting the dose can reduce dizziness and vomiting without losing pain control. But here’s where most people get it wrong: they think “splitting” means cutting a pill in half. That’s not the same thing. Cutting a pill is physical. Splitting a dose is pharmacological. One can save you money. The other can save your life-or land you in the ER.Tablet Splitting vs. Dose Splitting: Don’t Confuse Them
Tablet splitting is what you do with a knife or a pill cutter. You take a 20mg tablet, snap it in two, and take 10mg. Sounds simple, right? But if that tablet is designed to release the drug slowly over 12 hours, you’re breaking that system. You’re turning a controlled-release capsule into an instant shot of medicine. That spike? It’s now bigger and faster. And for drugs like extended-release tramadol or felodipine, that spike can cause dangerous drops in blood pressure, seizures, or even overdose. True dose splitting means taking the same total amount of medicine, but spread out. So instead of one 20mg pill once a day, you take two 10mg pills, 12 hours apart. This keeps the level in your blood more even. It’s not about cutting pills-it’s about timing. And it only works for certain kinds of drugs. The FDA says you should never split a tablet unless your doctor or pharmacist says it’s safe. And they’re not just being cautious. Between 2015 and 2020, over 1,200 adverse events in the U.S. were directly linked to people splitting pills they shouldn’t have. Nearly 40% of those involved blood thinners like warfarin. A tiny change in dose can cause a stroke or internal bleeding.Which Medications Can Be Safely Split?
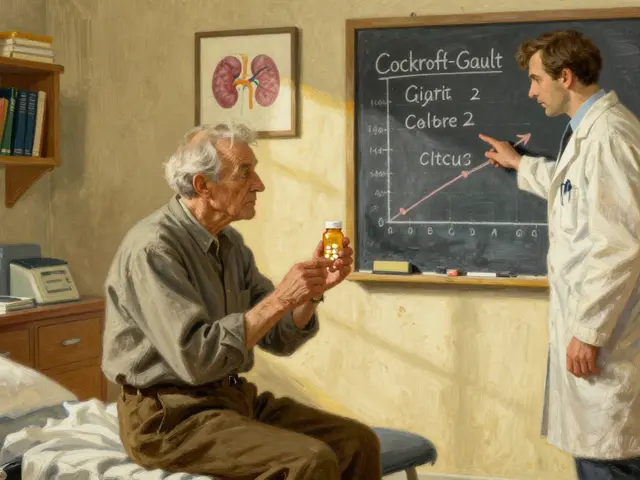
Not all drugs are created equal. Some have what’s called a wide therapeutic index-meaning there’s a big gap between a helpful dose and a harmful one. Acetaminophen, for example, has an index of about 10. You’d have to take a lot to overdose. These are safer candidates for dose adjustments. But drugs like digoxin or warfarin? Their therapeutic index is less than 2. That means a 10% change in dose can tip you from safe to dangerous. Splitting these? Don’t even think about it without medical supervision. Here’s what generally works for dose splitting:- Immediate-release formulations (not extended, delayed, or enteric-coated)
- Drugs with short half-lives (under 6 hours)
- Medications where side effects are tied to peak levels (not overall exposure)
- Therapeutic index above 3

Why Tablet Splitting Often Fails (And How to Do It Right)
Even if your doctor says it’s okay to split a tablet, most people do it wrong. Studies show that without proper training, 65% of patients end up with splits that vary by more than 15% in dose. That’s like taking 12mg instead of 10mg-or 8mg instead of 10mg. For a blood thinner, that’s a huge swing. The FDA recommends using a dedicated pill splitter-not a knife, not scissors. A good splitter can reduce dose variation to under 8%. Store split tablets in their original container, use them within a week, and keep them dry. Moisture can break down the drug or change how it’s absorbed. Also, not all scored tablets are safe to split. A 2020 analysis from the University of British Columbia found that unscored tablets had dose variability ranging from 80% to 120% of the intended amount. Even scored ones can vary by 5-15%. That’s why some manufacturers now test their scored tablets for uniformity-and if they fail, they’re required to label them “Do Not Split.” About 22% of scored tablets fall into this category.Cost vs. Safety: The Real Trade-Off
Let’s be honest. A lot of people split pills because they’re expensive. A 40mg atorvastatin tablet might cost $15. Two 20mg tablets? $30. But if you split the 40mg, you get two doses for $15. GoodRx says this saves patients up to $300 a year on statins alone. But here’s the hidden cost: if you split a pill you shouldn’t, and end up in the hospital because your INR spiked or your blood pressure crashed? That single ER visit can cost $3,000-$8,000. The FDA estimates inappropriate splitting could add $12.3 billion in avoidable healthcare costs each year in the U.S.-more than the $8.9 billion in savings from splitting. Pharmaceutical companies are catching on. Pfizer, for example, started making 5mg and 10mg versions of rivaroxaban after noticing a surge in people splitting 20mg tablets. Within a year, inappropriate splitting dropped by 78%. The message? If a drug is risky to split, make a lower dose. It’s safer, more reliable, and better for everyone.
When Dose Splitting Works Best: Real Cases
A 68-year-old woman in a 2023 NIH case report split a 40mg lisinopril tablet, thinking she was getting two 20mg doses. She didn’t realize the tablet wasn’t scored evenly. She ended up with 10mg one day and 30mg the next. Her blood pressure soared to 192/102. She had to be rushed to the hospital. Contrast that with a Reddit user who had chronic metformin diarrhea. They switched from 1000mg twice daily to 500mg four times daily. Diarrhea dropped from 60% of doses to 15%. No new meds. No extra cost. Just better timing. Another example: immediate-release stimulants for ADHD. Many patients feel jittery or anxious after a 20mg morning dose. Splitting into 10mg twice a day reduces that peak anxiety without losing focus. Same total dose. Smoother ride. The American Society of Health-System Pharmacists now lists 14 drug classes where dose splitting can reduce side effects-including immediate-release antipsychotics (for sedation), opioids (for nausea), and stimulants (for restlessness).What You Should Do Before You Split Anything
If you’re thinking about splitting your dose-whether for side effects or savings-follow this checklist:- Ask your pharmacist: “Is this tablet designed to be split?” Look for “Do Not Split” on the label.
- Confirm the formulation: Is it immediate-release? If it says “SR,” “ER,” “XL,” “CR,” or “XR,” don’t split it.
- Check the therapeutic index: If it’s for warfarin, digoxin, cyclosporine, or chemotherapy, don’t even consider it.
- Use a pill splitter, not a knife.
- Use split tablets within a week.
- Monitor for side effects or changes in symptoms for 5-7 days after changing your routine.
- Get a follow-up blood test if you’re on a drug with a narrow window (like warfarin or thyroid meds).
What’s Next?
Researchers are working on “smart pills” with engineered splitting lines that still preserve extended-release properties. Seven pharmaceutical companies have pending patents on this tech. But until then, the safest approach remains simple: if your doctor hasn’t specifically told you to split your dose, don’t. And if they have, make sure you understand exactly how-and why. The goal isn’t to cut pills. It’s to cut side effects. And sometimes, the best way to do that is to take less at a time-not to break the pill, but to break the habit of taking it all at once.Can I split my blood pressure pill to reduce dizziness?
Only if it’s an immediate-release version like lisinopril or hydrochlorothiazide. Never split extended-release versions like amlodipine Besylate or felodipine SR. Splitting those can cause dangerous drops in blood pressure. Always check the label for “ER,” “SR,” or “XL”-if it’s there, don’t split. Ask your pharmacist to confirm the formulation.
Is it safe to split metformin to stop stomach upset?
Yes, if it’s immediate-release metformin. Many patients successfully reduce nausea and diarrhea by splitting their total daily dose into smaller, more frequent doses-like 500mg four times a day instead of 1000mg twice. This avoids the high peak that irritates the gut. But if you’re on metformin ER (extended-release), do not split it. The coating is designed to release slowly; breaking it ruins that.
Why do some pills have a score line and others don’t?
A score line is just a groove-it doesn’t mean the pill is safe to split. It’s often there for manufacturing reasons or to make swallowing easier. The FDA now requires manufacturers to test scored tablets for dose uniformity. If they fail (meaning split pieces vary too much in drug content), they must label them “Do Not Split.” About 1 in 5 scored tablets fall into this risky category.
Can I save money by splitting my statin pill?
For immediate-release atorvastatin or simvastatin, yes-splitting a 40mg tablet to get two 20mg doses can save up to $300 a year. But only if your doctor approves it and the tablet is scored and safe to split. Never split extended-release statins or if you’re over 65, have kidney issues, or take other meds that interact. The cost savings aren’t worth the risk if you accidentally get too much or too little.
What if I accidentally split a pill I shouldn’t have?
Stop taking the split dose immediately. Call your pharmacist or doctor. If it’s a blood thinner, heart medication, or seizure drug, seek medical advice right away. Even if you feel fine, the dose you took might be too high or too low, and the effects could show up hours or days later. Don’t wait for symptoms. Get checked.
Are there any new alternatives to splitting pills?
Yes. More drugmakers are now producing lower-dose versions to avoid splitting altogether. For example, rivaroxaban now comes in 5mg and 10mg tablets instead of just 20mg. This cut inappropriate splitting by 78% in just one year. If you’re splitting because of cost, ask your doctor if a lower-dose option exists-it’s often safer and just as effective.




Comments(14)