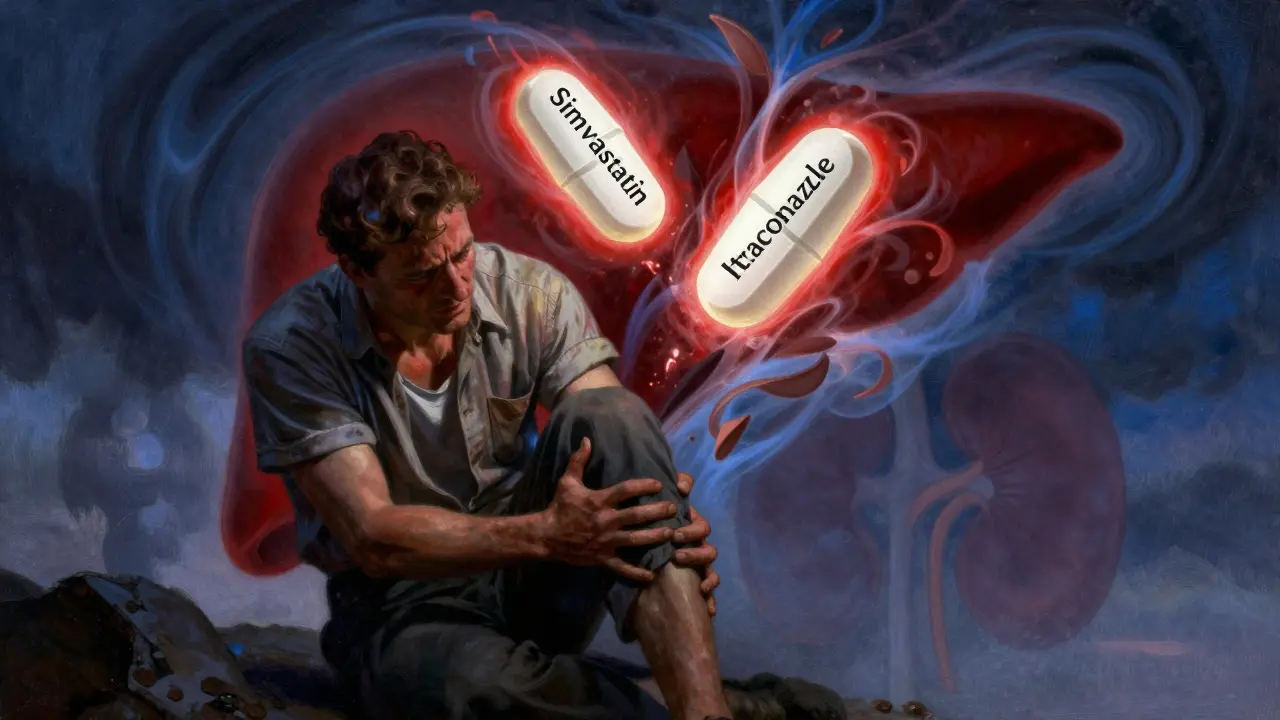
Imagine taking a pill for high cholesterol - something you’ve been on for years - and then getting a prescription for a fungal infection. Maybe it’s athlete’s foot, a yeast infection, or even a stubborn toenail fungus. You take both as directed. A few days later, your muscles feel like they’ve been run over by a truck. You can’t climb stairs. Your urine turns dark. That’s not just bad luck. That’s a dangerous, preventable drug interaction between statins and certain antifungals - and it’s happening more often than you think.
Why This Interaction Isn’t Just a Minor Warning
Statins are among the most prescribed drugs in the world. Over 300 million people take them to lower cholesterol and reduce heart attack risk. Common ones include atorvastatin, simvastatin, and rosuvastatin. Antifungals like fluconazole, itraconazole, and ketoconazole are used to treat everything from ringworm to life-threatening fungal infections. On the surface, they seem unrelated. But inside your body, they collide. The problem lies in how your liver breaks down these drugs. Most statins are processed by enzymes called CYP3A4 and CYP2C9. Azole antifungals - especially itraconazole and ketoconazole - are powerful blockers of these same enzymes. When you take them together, your liver can’t clear the statin fast enough. The statin builds up. And when it builds up too much, it starts tearing down muscle tissue. This isn’t theoretical. In 2016, a case report in the BMJ documented a patient who developed rhabdomyolysis - a condition where muscle breaks down so badly it floods the kidneys with toxic proteins - after taking simvastatin and itraconazole together. His muscle enzyme levels (CK) spiked to over 15,000 U/L. Normal is under 200. He needed emergency dialysis. He survived. Many don’t.Which Statins Are Riskiest?
Not all statins are created equal when it comes to drug interactions. Here’s the reality:- High risk: Simvastatin and lovastatin. These are metabolized almost entirely by CYP3A4. Taking them with itraconazole or ketoconazole can raise their levels by 10 times or more. The FDA explicitly says: Do not combine simvastatin with itraconazole.
- Moderate risk: Atorvastatin. Also processed by CYP3A4. Dose must be capped at 20 mg per day if you’re on a strong azole antifungal. Even then, monitor closely.
- Low risk: Pravastatin and rosuvastatin. These barely touch CYP enzymes. Most are removed unchanged by the kidneys. If you need an antifungal, these are your safest options.
- Special case: Fluvastatin. Metabolized by CYP2C9, so fluconazole (which inhibits this enzyme) can still cause issues - but less severely than with simvastatin.
If you’re on simvastatin and your doctor prescribes itraconazole for a fungal nail infection, that’s a red flag. Not a suggestion. A warning. And if you’re on atorvastatin and get a prescription for voriconazole - common in hospital-treated fungal infections - your dose needs to be reviewed immediately.
The Hidden Benefit: Statins Might Fight Fungi Too
Here’s the twist: while these drugs can be dangerous together, they might also work better together - in a good way. Studies show that statins, especially fluvastatin and atorvastatin, have their own antifungal properties. They interfere with cholesterol-like molecules in fungal cell membranes. When paired with azoles - which attack the same pathway - they can team up to kill resistant fungi like Candida auris, a deadly, drug-resistant yeast that’s spread rapidly in hospitals since 2020. A 2023 study found that rosuvastatin and voriconazole worked together against C. auris in 40-60% of lab samples. No antagonism. Just synergy. Researchers are now running clinical trials (NIH trial NCT05678912) to see if low-dose statins can help treat stubborn fungal infections in high-risk patients. But here’s the catch: this benefit only matters in controlled, monitored settings. You can’t just start taking your cholesterol pill with your antifungal and hope for the best. The dose window for synergy is narrow. The risk of muscle damage is wide.
What You Should Do Right Now
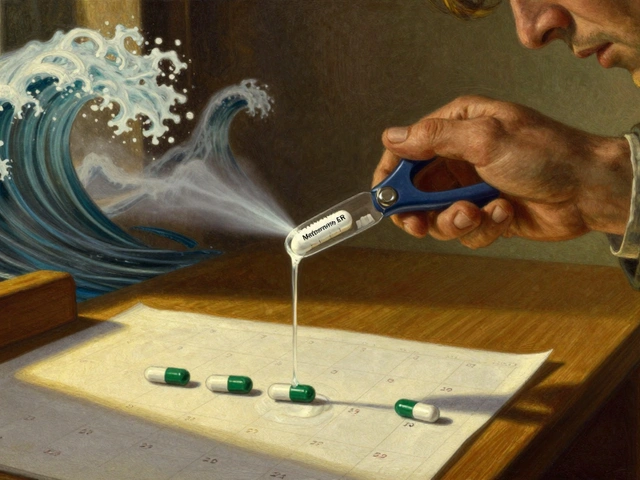
If you’re on a statin and your doctor is about to prescribe an antifungal, here’s what you need to do:- Ask: Is this infection confirmed? Many people get antifungals for rashes or itching that aren’t fungal at all. Get a culture if possible. Topical treatments (creams, sprays) are often enough for skin or nail infections - and they don’t enter your bloodstream.
- Ask: Is there a safer antifungal? Terbinafine (Lamisil) doesn’t interact with statins. It’s often just as effective for toenail fungus. Ask if it’s an option.
- Ask: Can I switch statins? If you’re on simvastatin or lovastatin, ask if you can switch to pravastatin or rosuvastatin during your antifungal treatment. Most patients do this safely. Cholesterol levels stay stable.
- Ask: Should I pause my statin? For high-risk combinations (like simvastatin + itraconazole), stopping the statin 2 days before and 2 days after the antifungal can prevent toxicity. This isn’t guesswork - it’s a proven protocol from clinical case studies.
Don’t wait for symptoms. Muscle pain, weakness, or dark urine are late signs. By then, damage may already be done. Talk to your pharmacist. They’re trained to catch these interactions. In fact, one pharmacist on Reddit said they’ve caught 12 dangerous statin-azole combos in just one quarter.
What Doctors Don’t Always Tell You
A 2023 study in JAMA Internal Medicine found only 42% of primary care doctors could correctly identify which statin-azole pairs were dangerous. That’s not your fault. It’s a system problem. Many doctors focus on the heart disease. The antifungal feels like a side issue. But when you’re on both, the antifungal becomes the bigger threat. The American College of Cardiology issued a clinical alert in 2021: Avoid simvastatin, lovastatin, and high-dose atorvastatin with strong CYP3A4 inhibitors. Yet, these combinations still happen - often because the patient didn’t mention they were taking both, or the pharmacist didn’t flag it. Electronic health systems are getting better. Epic Systems added interaction alerts in their 2024 update. But if your doctor’s office hasn’t upgraded yet? You’re on your own.



Comments(14)