Antifungals: What They Are, How They Work, and What You Need to Know
When your skin itches, your nails thicken, or you get recurring yeast infections, you’re likely dealing with a fungus, a type of microorganism that thrives in warm, moist areas of the body and can cause persistent, uncomfortable infections. Also known as yeast or mold, these organisms aren’t bacteria—they need different tools to fight them. That’s where antifungals, medications designed specifically to kill or slow the growth of fungi come in. Unlike antibiotics that target bacteria, antifungals work by breaking down the fungal cell wall or blocking its ability to reproduce. They’re not optional for serious cases—they’re necessary.
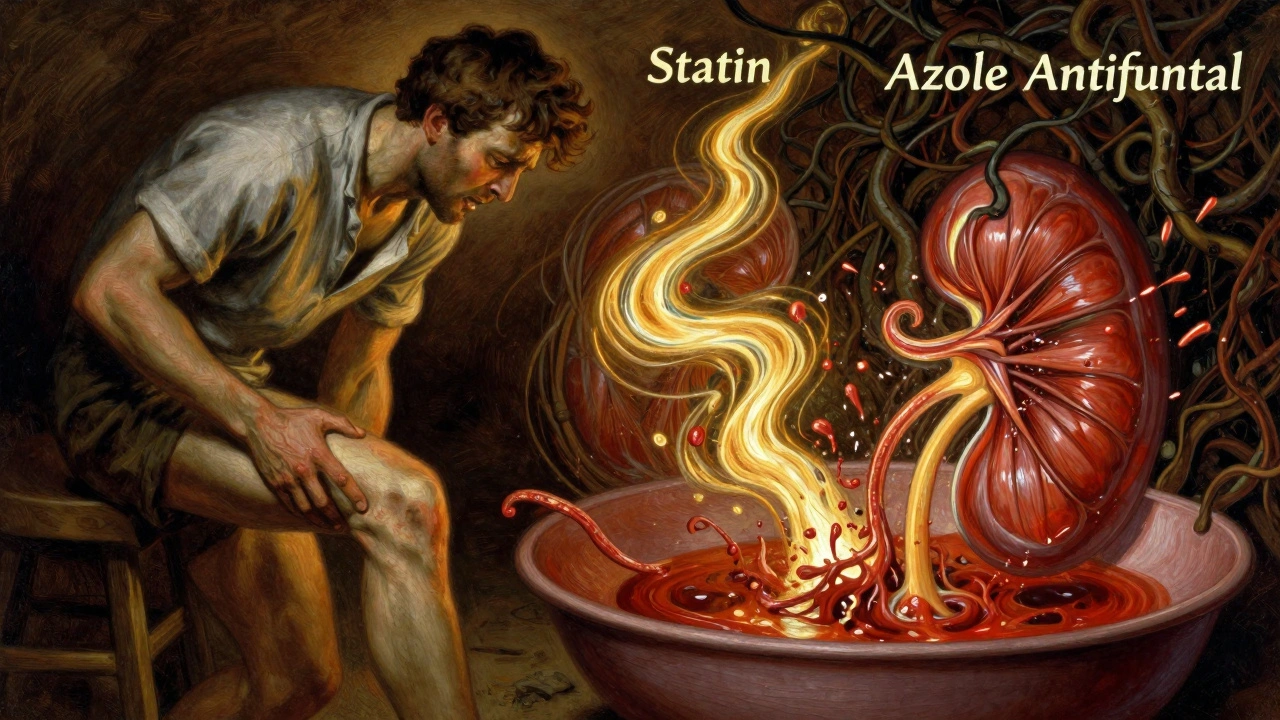
Not all antifungals are the same. Some, like clotrimazole or miconazole, are creams or sprays you apply directly to the skin for athlete’s foot or ringworm. Others, like fluconazole or itraconazole, are pills that treat deeper infections like vaginal yeast infections or oral thrush. For life-threatening cases—like fungal pneumonia in immunocompromised patients—doctors use stronger IV antifungals like amphotericin B. What matters most is matching the drug to the infection type and location. Using the wrong one won’t help, and using it too long can cause liver damage or disrupt your gut bacteria. Many people don’t realize that even over-the-counter antifungals can interact with other meds. For example, ketoconazole can mess with cholesterol drugs, and terbinafine can affect how your body processes antidepressants. Always check with your pharmacist before starting anything new.
There’s also a growing concern about antifungal resistance. Just like with antibiotics, overuse and incomplete courses are making some fungi harder to treat. If you’ve had the same yeast infection three times in a year, it might not be bad luck—it could be resistance. And while natural remedies like coconut oil or tea tree oil get talked about online, there’s little solid evidence they work as well as prescription antifungals. The real winners are the ones backed by clinical trials: fluconazole for yeast, terbinafine for nail fungus, and topical azoles for skin. What you’ll find below are real, practical posts that break down how these drugs work, what side effects to watch for, how to avoid mistakes, and when to push back if your treatment isn’t working. No fluff. No guesswork. Just what you need to know to get better—and stay better.