Statin-Antifungal Interaction Checker
Check if your statin and antifungal combination is safe. This tool uses FDA guidelines and clinical evidence to show interaction risks and provide safe alternatives.
When you take a statin to lower cholesterol and an antifungal to treat a stubborn yeast infection, you might think you’re just managing two separate health issues. But behind the scenes, these two medications can collide in a way that puts your muscles at serious risk. The result? A rare but life-threatening condition called rhabdomyolysis-where muscle tissue breaks down so fast that it floods your bloodstream with toxic proteins, potentially causing kidney failure or even death.
Why This Interaction Isn’t Just a Warning on a Label
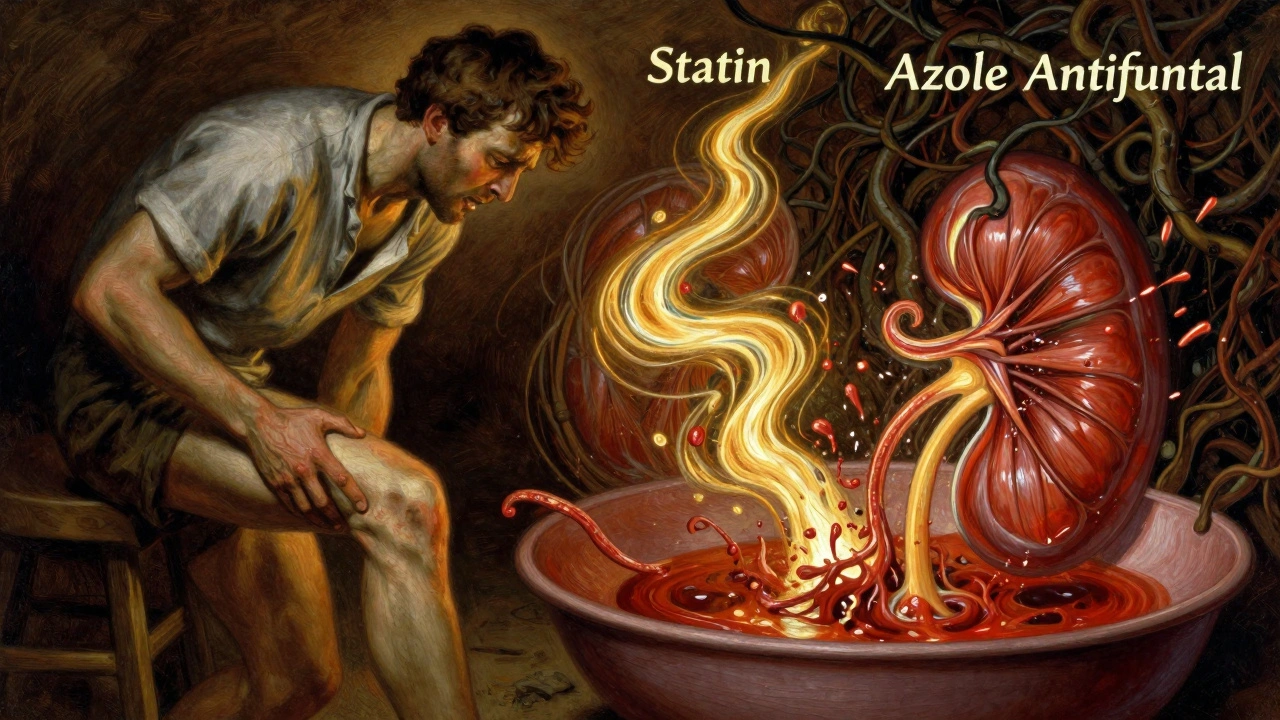
Statins like simvastatin, lovastatin, and atorvastatin work by blocking an enzyme in your liver that makes cholesterol. But they also rely on a liver enzyme called CYP3A4 to break them down and get them out of your system. That’s where antifungals come in. Azole antifungals-such as itraconazole, voriconazole, and ketoconazole-are designed to kill fungi by interfering with their cell membranes. But they’re also powerful inhibitors of CYP3A4. When you take them together, they essentially shut down the main exit route for your statin.This isn’t theoretical. In 2012, the FDA strengthened its warning labels after reviewing dozens of cases where patients on simvastatin developed rhabdomyolysis after starting itraconazole. One study found that when someone took simvastatin with itraconazole, the amount of active statin in their blood jumped by more than 10 times. That’s not a small increase-it’s the difference between a safe dose and a toxic one.
Not All Statins Are Created Equal
If you’re on a statin and need an antifungal, not all statins carry the same risk. Some are like gas-guzzling trucks-dependent on CYP3A4 to clear them. Others are more like electric cars-they don’t rely on that pathway at all.- High-risk statins: Simvastatin, lovastatin, and atorvastatin. These are metabolized mostly by CYP3A4. Simvastatin is the worst offender. Even a low dose of 20 mg can become dangerous when paired with itraconazole.
- Low-risk statins: Pravastatin, fluvastatin, rosuvastatin, and pitavastatin. These use different enzymes (like CYP2C9 or just direct excretion) and aren’t significantly affected by azole antifungals.
For example, if you’re on simvastatin 40 mg and get prescribed fluconazole for a vaginal yeast infection, your risk of muscle damage goes up by 22 times compared to taking simvastatin alone. But if you switch to pravastatin 40 mg, your risk stays nearly the same as if you weren’t taking the antifungal at all.
The Real-World Cost of Overlooking This
This isn’t just a lab curiosity. Between 2010 and 2019, the FDA’s own database recorded over 1,200 cases of rhabdomyolysis linked to statin-azole combinations. Simvastatin and itraconazole made up nearly 40% of those cases. Fluconazole, which many doctors think is "safer," was involved in almost 30%.Real patients are getting hurt. A 68-year-old man in a 2018 case report developed rhabdomyolysis after just seven days on simvastatin 40 mg and fluconazole 200 mg daily for toenail fungus. His creatine kinase (CK) levels-normally under 200 U/L-shot up to 18,400 U/L. He was hospitalized for three days. He didn’t have kidney failure, but he came close.
On Reddit, pharmacists report seeing 2-3 cases per year in their practices. Most involve older adults with diabetes, high blood pressure, or kidney issues-people who are already more vulnerable. Often, the antifungal was prescribed by a dermatologist or gynecologist who didn’t know the patient was on a statin. Or worse, the patient didn’t tell them.
What the Guidelines Say-And What Doctors Still Miss
The FDA says this clearly: Do not use simvastatin above 20 mg with itraconazole, ketoconazole, or posaconazole. Avoid simvastatin entirely with voriconazole. For fluconazole, max simvastatin dose is 10 mg per day. Atorvastatin max is 20 mg with fluconazole.But here’s the problem: a 2022 study found that nearly 19% of patients still got these dangerous combinations. That number jumped to 23% for patients over 75. Why? Because prescriptions are often written in different systems. A primary care doctor prescribes the statin. A dermatologist prescribes the antifungal. Neither checks the other’s list. And many patients don’t know to tell both doctors.
Hospitals have gotten better. Systems like Epic now have hard stops-they won’t let a pharmacist fill a simvastatin 80 mg prescription if itraconazole is on file. But in outpatient clinics? The warnings are still soft. Many prescriptions go through unchecked.
What You Should Do Right Now
If you’re taking a statin and your doctor prescribes an antifungal, don’t wait. Ask these questions:- Is this antifungal an azole? (Itraconazole, ketoconazole, voriconazole, fluconazole, posaconazole-yes, all are.)
- Which statin am I on? (Simvastatin? Lovastatin? Atorvastatin?)
- Can we switch to a safer statin like pravastatin or rosuvastatin?
- If we must keep this combination, what’s the lowest safe dose?
Don’t assume your pharmacist caught it. Pharmacists are stretched thin. You’re your own best advocate.
Alternatives That Actually Work
You don’t have to choose between managing cholesterol and treating a fungal infection. There are safer paths:- Switch your statin: Pravastatin 40 mg, fluvastatin 80 mg, or rosuvastatin 20 mg are all safe with azoles. Rosuvastatin is especially effective for high LDL and doesn’t interact.
- Switch your antifungal: Isavuconazole, approved in 2015, barely touches CYP3A4. It’s not used for simple yeast infections, but for serious fungal pneumonia or systemic infections, it’s a game-changer. Terbinafine, another antifungal, doesn’t inhibit CYP3A4 at all-great for nail fungus.
- Time it right: If you absolutely must take simvastatin with fluconazole, keep the dose at 10 mg or less. Stop the statin 2-3 days before starting the antifungal, and wait 2-3 days after finishing the antifungal before restarting the statin.
Watch for These Symptoms
Rhabdomyolysis doesn’t come on suddenly. It creeps up. The first signs are subtle:- Severe muscle pain, especially in the thighs, shoulders, or lower back
- Unexplained weakness-you can’t climb stairs or lift your arms
- Dark, tea-colored urine (this is a red flag-your muscles are breaking down)
If you notice any of these while taking both drugs, stop the statin immediately and call your doctor. Don’t wait for the pain to get worse. A simple blood test for creatine kinase can catch this before it turns into kidney failure.
The Bigger Picture: Why This Keeps Happening
This isn’t just about two drugs. It’s about how fragmented healthcare is. Patients see specialists who focus on one thing-cholesterol, or a fungal rash. Few systems automatically check for interactions across different providers. And many patients don’t know their meds are interacting because they’re not told.But progress is happening. Between 2015 and 2022, rhabdomyolysis cases from this interaction dropped by 34% thanks to EHR alerts, pharmacist-led reviews, and better education. That’s proof that awareness saves lives.
If you’re on a statin and need an antifungal, don’t let silence be your default. Ask. Double-check. Push for safer options. Your muscles-and your kidneys-depend on it.
Can fluconazole really cause rhabdomyolysis with statins?
Yes. While fluconazole is a weaker CYP3A4 inhibitor than itraconazole or ketoconazole, it still significantly increases statin levels. Studies show fluconazole 200 mg/day can raise simvastatin exposure by 350% and atorvastatin by 80%. Cases of rhabdomyolysis have been documented in patients taking fluconazole with simvastatin, even at 20 mg daily. The FDA recommends capping simvastatin at 10 mg daily when combined with fluconazole.
Is it safe to take pravastatin with any antifungal?
Yes. Pravastatin is metabolized mainly through non-CYP3A4 pathways, so it doesn’t build up dangerously when taken with azole antifungals like fluconazole, itraconazole, or voriconazole. Clinical studies show no significant increase in muscle toxicity risk. Pravastatin 40 mg daily is considered a safe alternative for patients needing long-term antifungal therapy.
What if I’m on simvastatin and need an antifungal for a fungal nail infection?
Don’t take simvastatin while on antifungals for nail fungus. Even a 12-week course of fluconazole or terbinafine can trigger rhabdomyolysis. Switch to pravastatin or rosuvastatin before starting the antifungal. If switching isn’t possible, stop simvastatin during treatment and restart only after the antifungal course ends and you’ve waited 2-3 days. Always check with your doctor before making changes.
Are there any new antifungals that don’t interact with statins?
Yes. Isavuconazole, approved by the FDA in 2015, has minimal effect on CYP3A4 and shows no clinically significant interaction with simvastatin in trials. It’s not used for simple infections like yeast or nail fungus, but for serious systemic fungal diseases, it’s a safer choice than itraconazole or voriconazole. Terbinafine, often used for nail fungus, also doesn’t inhibit CYP3A4 and is safe with all statins.
How do I know if I’m at higher risk for this interaction?
You’re at higher risk if you’re over 65, have kidney disease, diabetes, or take multiple medications. People with a genetic variant called CYP3A5*3/*3 (poor metabolizers) are 2.3 times more likely to develop toxicity when statins and azoles are combined. If you’ve had muscle pain or elevated CK levels on statins before, you’re also at higher risk. Always tell your doctor your full medication list-including supplements and OTC drugs.
If you’re on a statin and your doctor prescribes an antifungal, ask: "Is this safe with my cholesterol med?" If they’re unsure, ask them to check a drug interaction checker or consult a pharmacist. This interaction is preventable-but only if you speak up.



Comments(12)