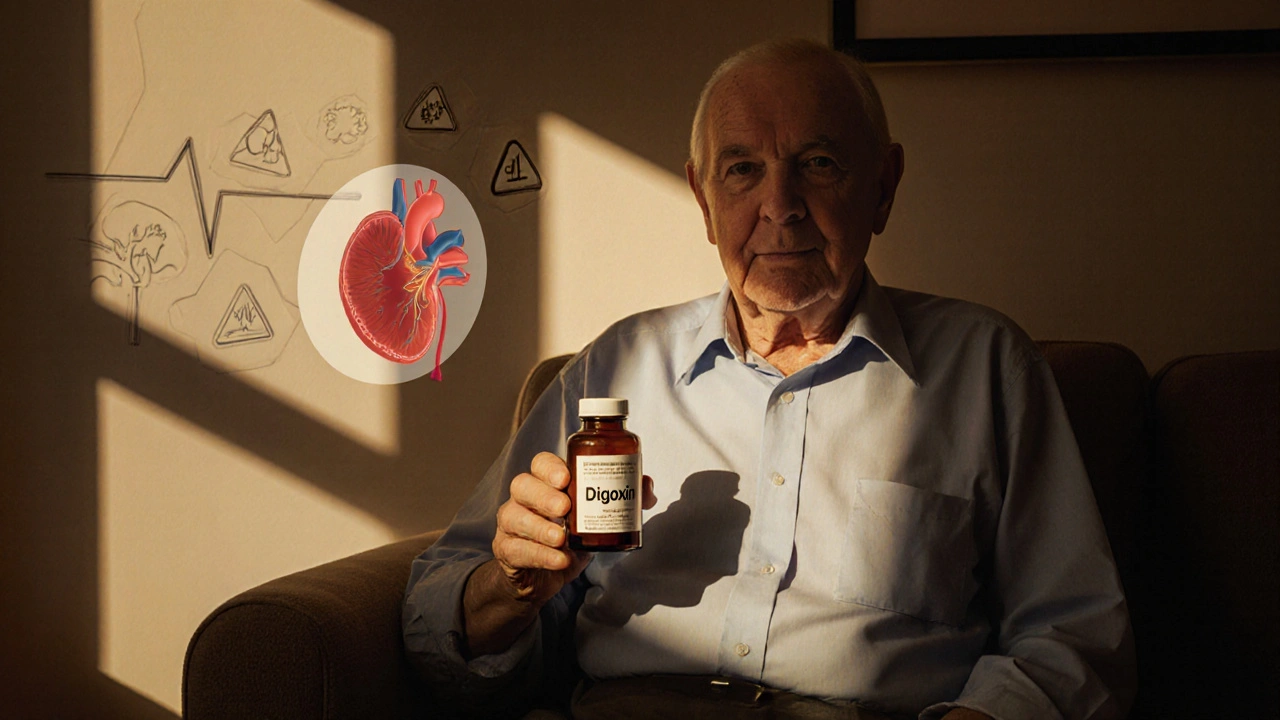
Digoxin: Uses, Risks, and Alternatives for Heart Conditions
When your heart struggles to pump efficiently, digoxin, a cardiac glycoside derived from the foxglove plant, used for decades to strengthen heart contractions and slow rapid heart rates. Also known as digitalis, it’s one of the oldest heart medications still in use today. Unlike newer drugs, digoxin doesn’t improve survival rates—but it can ease symptoms like shortness of breath and fatigue in people with heart failure, a condition where the heart can’t pump enough blood to meet the body’s needs. It’s also commonly prescribed for atrial fibrillation, an irregular heartbeat that raises stroke risk, because it helps control how fast the heart beats.
But digoxin is tricky. The difference between a helpful dose and a dangerous one is small. Too much can cause nausea, confusion, vision changes, or even life-threatening heart rhythms. Older adults, people with kidney problems, or those taking other medications like diuretics or antibiotics are at higher risk. That’s why doctors monitor blood levels closely and often avoid it unless other treatments haven’t worked. Many patients now get better results with beta-blockers, drugs that reduce heart rate and blood pressure or ACE inhibitors, which relax blood vessels and reduce strain on the heart. These are safer, more effective for long-term use, and often improve survival.
If you’re on digoxin, you’re not alone—but you should know your options. The posts below cover real cases: why some people switch away from digoxin, how it interacts with common supplements like magnesium or potassium, what to watch for if you’re elderly, and how newer drugs compare in cost, safety, and results. You’ll find practical advice from people managing heart conditions at home, tips for avoiding dangerous drug combos, and clear comparisons with alternatives that work better today. This isn’t just about a drug—it’s about making smarter choices for your heart.