When doctors talk about treating heart failure, digoxin often comes up - not because it’s the first choice anymore, but because it still has a place in the toolbox. It’s an old drug, used for over 200 years, and yet it hasn’t disappeared from hospitals or prescriptions. Why? Because for some patients, it works. But it’s not without risks. If you or someone you know is on digoxin, or being considered for it, you need to know what it really does - and what it might do to you.
What digoxin actually does in the heart
Digoxin is a cardiac glycoside. That’s a fancy way of saying it comes from the foxglove plant and affects how heart muscle cells handle calcium. It slows down the heart rate slightly and makes each beat stronger. This helps when the heart is weak and struggling to pump blood efficiently. Unlike newer drugs like beta-blockers or ACE inhibitors that change how the body handles fluid and pressure, digoxin works directly on the heart muscle.
It’s not a cure. It doesn’t extend life the way some other heart failure meds do. But it does reduce hospital visits. In clinical trials, patients on digoxin had about 20% fewer hospitalizations for worsening heart failure. That matters - because hospital stays for heart failure are expensive, exhausting, and dangerous.
The real benefits: when digoxin helps
Digoxin isn’t for everyone. But for certain groups, it’s one of the few tools left that still works well.
- People with atrial fibrillation and heart failure: If your heart is beating irregularly and weakly, digoxin helps control the rate. It doesn’t fix the rhythm, but it keeps it from racing out of control, which reduces symptoms like dizziness and shortness of breath.
- Patients who can’t tolerate other drugs: Some people develop kidney problems, low blood pressure, or severe coughs from ACE inhibitors or ARBs. Digoxin doesn’t cause those side effects, so it becomes a fallback option.
- Those with persistent symptoms despite standard therapy: Even if you’re on beta-blockers, diuretics, and SGLT2 inhibitors, you might still feel tired and swollen. Digoxin can add a small but meaningful boost in how you feel day to day.
It’s not magic. But for about 10-15% of heart failure patients who still struggle after trying everything else, digoxin can make the difference between being stuck at home and being able to walk to the mailbox.
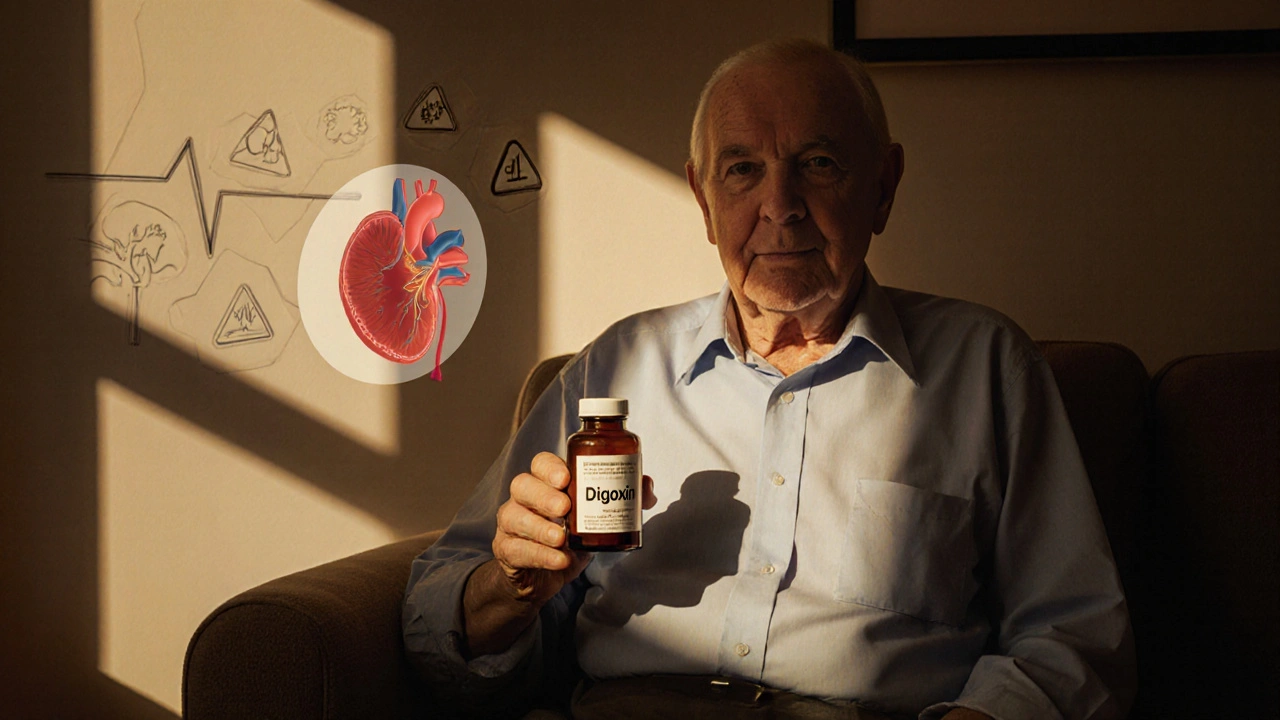
The hidden dangers: why digoxin scares doctors
Digoxin has a very narrow safety window. That means the dose that helps is almost the same as the dose that poisons you. A few milligrams too much - or a little dehydration, or a change in kidney function - can push you into toxicity.
Signs of digoxin toxicity include:
- Nausea, vomiting, loss of appetite
- Blurred vision or yellow-green halos around lights
- Confusion, dizziness, fatigue
- Irregular heartbeat - sometimes dangerously slow, sometimes dangerously fast
These aren’t rare. Studies show up to 25% of patients on digoxin have some level of toxicity, especially if they’re older or have kidney disease. And because symptoms mimic other conditions - like the flu or aging - many cases go missed until it’s too late.
Older adults are especially at risk. Their kidneys don’t clear digoxin as well. Their bodies hold onto it longer. And many are taking other meds - like antibiotics or diuretics - that interact badly with it. One study found that nearly half of digoxin-related ER visits in people over 65 were preventable.

Monitoring: what you need to do if you’re on digoxin
If you’re prescribed digoxin, you’re not just taking a pill. You’re entering a monitoring program.
Here’s what you need:
- Regular blood tests: Your doctor should check your digoxin level every 3-6 months, or anytime your health changes. The safe range is 0.5 to 0.9 ng/mL. Above 1.2? You’re in danger zone.
- Electrolyte checks: Low potassium or magnesium makes digoxin toxicity way more likely. Your doctor should test these at least every 3 months.
- Kidney function tests: Digoxin is cleared by the kidneys. If your creatinine rises, your dose needs to drop - fast.
- Medication review: Many common drugs - like amiodarone, verapamil, and even some antibiotics - raise digoxin levels. Always tell every new doctor you’re on digoxin.
And if you feel off - even a little - don’t wait. Call your doctor. Don’t assume it’s just aging or stress. Digoxin toxicity can turn deadly in hours.
How digoxin stacks up against modern heart failure drugs
There’s been a revolution in heart failure treatment since the 1990s. New drugs like sacubitril/valsartan (Entresto), SGLT2 inhibitors (Farxiga, Jardiance), and vericiguat have proven they save lives. They reduce death by 20-30%. Digoxin? It doesn’t do that.
Here’s the reality:
| Drug | Reduces Death? | Reduces Hospitalizations? | Requires Monitoring? | Common Side Effects |
|---|---|---|---|---|
| Digoxin | No | Yes (modest) | Yes (frequent) | Nausea, vision changes, arrhythmias |
| SGLT2 Inhibitors (e.g., Farxiga) | Yes (up to 30%) | Yes (up to 30%) | Minimal | Genital yeast infections, mild dehydration |
| Entresto (sacubitril/valsartan) | Yes (20%) | Yes (20%) | Yes (blood pressure) | Dizziness, low blood pressure, cough |
| Beta-blockers (e.g., carvedilol) | Yes (30-35%) | Yes (30%) | Yes (heart rate, blood pressure) | Fatigue, low heart rate, depression |
Modern drugs are safer, more effective, and easier to manage. That’s why guidelines now put digoxin at the bottom of the list - only after the big four: beta-blockers, ACE inhibitors/ARBs/ARNIs, SGLT2 inhibitors, and mineralocorticoid antagonists.
Who should avoid digoxin entirely?
Digoxin isn’t safe for everyone. Avoid it if you:
- Have ventricular tachycardia or certain types of heart block (unless you have a pacemaker)
- Have severe kidney disease (eGFR under 30) without dose adjustment
- Are allergic to cardiac glycosides
- Have low potassium or magnesium levels that can’t be corrected
- Are taking drugs like clarithromycin, itraconazole, or cyclosporine - they spike digoxin levels dangerously
Also, don’t start digoxin if you’re over 80 and have no atrial fibrillation. The risks almost always outweigh the benefits in that group.
Is digoxin worth it in 2025?
Yes - but only in very specific cases.
If you have heart failure with atrial fibrillation and you’re still symptomatic despite taking all the modern drugs, digoxin can help you feel better. It’s not glamorous. It’s not life-saving. But it can improve your quality of life - if you’re monitored closely.
For most people, though, it’s outdated. If you’re newly diagnosed with heart failure, you should be on a combination of newer drugs first. Digoxin is not the starting point anymore. It’s the backup plan.
And if you’re already on it? Don’t stop. But ask your doctor: Why am I still on this? Is it helping? Are we checking my levels? Are there safer options now? You deserve to be on the best, safest treatment possible.
Can digoxin cause weight gain?
Digoxin itself doesn’t cause weight gain. But if it’s not working well, your heart failure may worsen, leading to fluid retention and swelling - which can show up as sudden weight gain. If you notice rapid weight gain (more than 2-3 pounds in a day), contact your doctor. It’s not the digoxin causing it - it’s your heart.
Is digoxin safe for elderly patients?
It can be - but only with extreme caution. Older adults are more sensitive to digoxin because their kidneys clear it slower. Doses are often cut in half. Blood levels must be checked regularly. Many doctors avoid it in people over 75 unless absolutely necessary. If you’re elderly and on digoxin, ask if your dose is appropriate and if you’re getting tested often enough.
Can I take digoxin with vitamin D or calcium supplements?
Not without your doctor’s approval. High calcium levels can increase the risk of digoxin toxicity. Vitamin D raises calcium levels in the blood. If you’re taking either, your doctor needs to know. They may need to lower your digoxin dose or monitor you more closely.
Does digoxin interact with over-the-counter meds?
Yes. Even common OTC drugs like antacids, laxatives, and some herbal supplements (like St. John’s Wort) can interfere. Antacids can reduce digoxin absorption. Laxatives can lower potassium, increasing toxicity risk. Always check with your pharmacist before taking anything new.
How long does it take for digoxin to start working?
You might notice a change in your heart rate within a few hours, especially if you have atrial fibrillation. But it takes 5-7 days for the full effect on heart failure symptoms like swelling and fatigue. Don’t expect instant relief. And don’t increase the dose if you don’t feel better right away - that’s how toxicity starts.
What to do next if you’re on digoxin
First, don’t panic. Digoxin isn’t evil - it’s just old and finicky. But it’s not the future of heart failure care.
Here’s your action plan:
- Get your digoxin blood level checked - if it’s been over 6 months, schedule it now.
- Ask your doctor if you’re on the lowest effective dose. Many people are on too much.
- Review all your medications - including supplements - with your pharmacist.
- Ask: Is there a newer drug I could try instead? Even if you feel okay, newer options might be safer long-term.
- Keep a symptom diary: note swelling, fatigue, dizziness, appetite changes. Bring it to every appointment.
Digoxin has a role - but only if it’s used carefully, monitored closely, and never assumed to be the best option. In 2025, heart failure treatment is smarter than it’s ever been. You deserve to be on the right drug - not just the one that’s been around the longest.






Comments(13)