Pregnancy Safety: What Medications Are Safe and What to Avoid
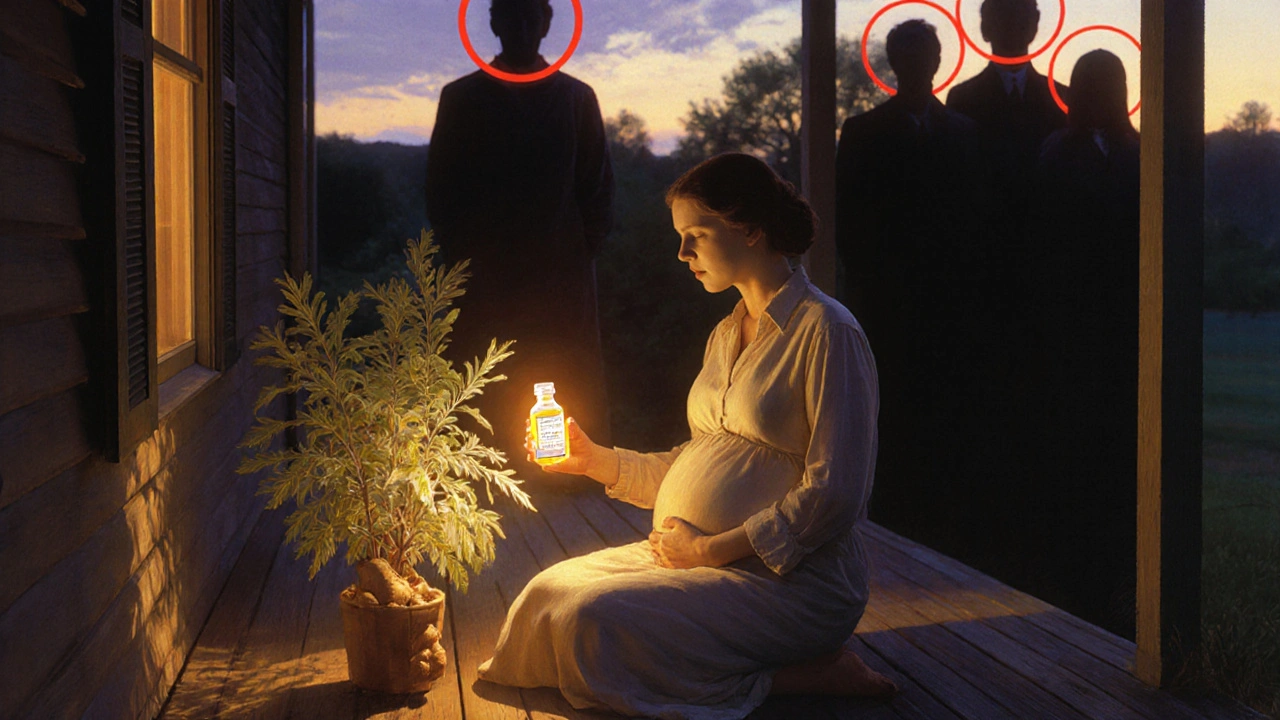
When you're pregnant, every pill, supplement, or cold remedy becomes a decision with two lives in mind. Pregnancy safety, the practice of choosing treatments that protect both mother and developing baby. Also known as prenatal medication safety, it’s not about avoiding all drugs—it’s about knowing which ones truly help and which ones carry hidden risks. Many women assume that if a drug is sold over the counter, it’s safe. But that’s not true. Even common painkillers like ibuprofen or aspirin can affect fetal development, especially in later stages. The same goes for some antibiotics, antidepressants, and herbal supplements you might think are harmless.
It’s not just about what you take—it’s about what your body does with it. Some medications cross the placenta easily and can interfere with organ development, especially in the first trimester. Others build up over time and affect blood flow or hormone levels. For example, antibiotics like tetracycline, a class of drugs that can permanently stain a baby’s teeth and affect bone growth, are strictly avoided after the first trimester. Meanwhile, acetaminophen, the most commonly recommended pain reliever during pregnancy, is considered low-risk when used at the right dose and duration. But even that has limits—long-term or high-dose use has been linked to developmental concerns in some studies.
Managing chronic conditions during pregnancy adds another layer. If you have diabetes, epilepsy, high blood pressure, or depression, stopping your meds can be just as dangerous as taking the wrong ones. That’s why working with your doctor to switch to safer alternatives—like switching from lisinopril to methyldopa for blood pressure, or from SSRIs with higher risks to ones like sertraline—is critical. Many women don’t realize that untreated conditions often pose a bigger threat than the medications used to treat them.
And it’s not just pills. Some topical creams, essential oils, and even prenatal vitamins with too much vitamin A can be risky. You might think natural equals safe, but that’s a myth. Herbal teas like black cohosh or dong quai can trigger contractions. Fish oil is fine, but high-dose vitamin A supplements aren’t. The line between helpful and harmful isn’t always clear—and that’s why reliable, evidence-based guidance matters more than ever.
Below, you’ll find real-world advice from women who’ve navigated these choices, doctors who’ve seen the consequences of misinformation, and studies that cut through the noise. Whether you’re trying to conceive, in your first trimester, or nearing delivery, these posts give you the facts—not fear—so you can make confident, informed decisions. No guesswork. No fluff. Just what you need to keep yourself and your baby safe.