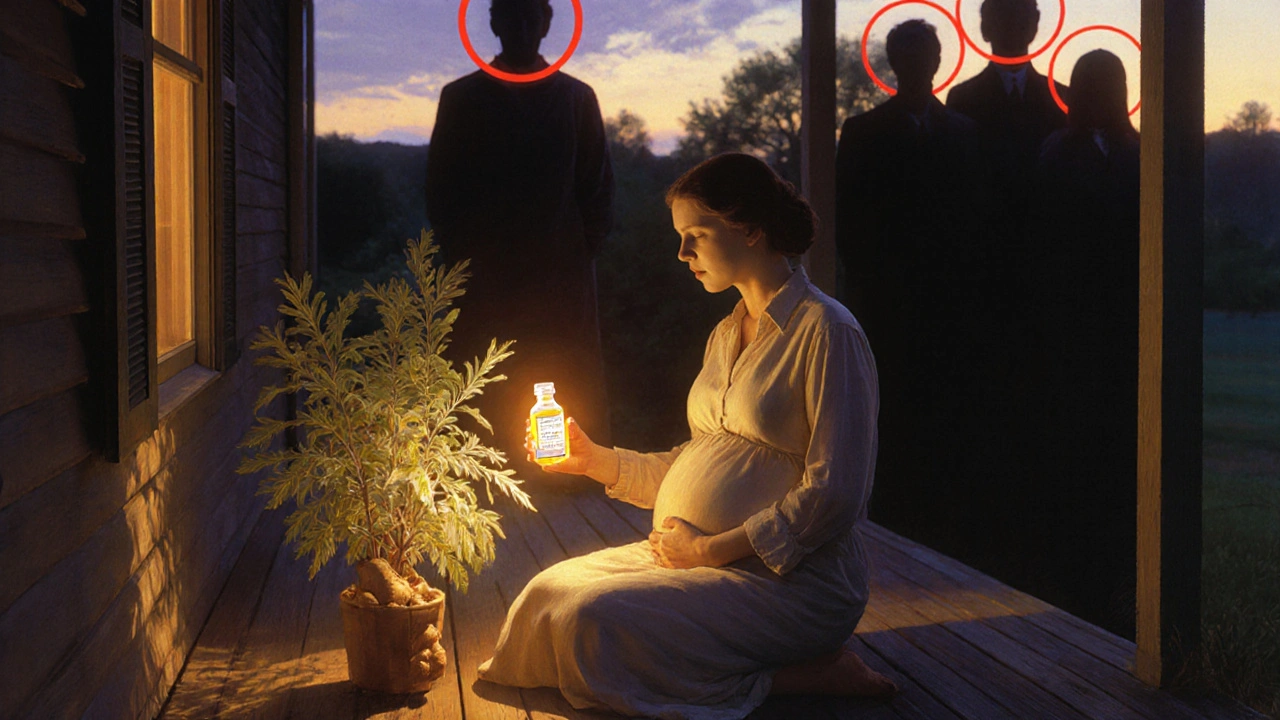
More than 1 in 4 pregnant women take herbal supplements. Not because they’re reckless, but because they’re told these are "natural" and therefore safe. The truth? It’s not that simple. While some herbs like ginger might help with morning sickness, others could trigger spotting, preterm labor, or even affect your baby’s heart. And here’s the scary part: most of these products aren’t tested for pregnancy safety at all.
Why Herbal Supplements Are a Wild Card in Pregnancy
Pregnant women turn to herbal supplements for all kinds of reasons-nausea, trouble sleeping, urinary infections, or just because their mom swore by chamomile tea. But unlike prescription drugs, herbal products don’t have to prove they’re safe before hitting store shelves. The FDA doesn’t review them for safety, effectiveness, or even consistent dosing. That means one bottle of raspberry leaf might have 200 mg of active compounds, and the next could have 800 mg-or worse, unlisted contaminants like heavy metals or even prescription drugs. This lack of oversight isn’t just a loophole; it’s a gap in care. Studies show 20% to 60% of herbal supplements contain ingredients not listed on the label. Some have fillers, pesticides, or even banned substances. And because pregnant women are almost never included in clinical trials, we’re flying blind. We don’t know how most herbs affect fetal development, placental function, or long-term child outcomes.What Herbs Are Actually Studied-and What’s Risky
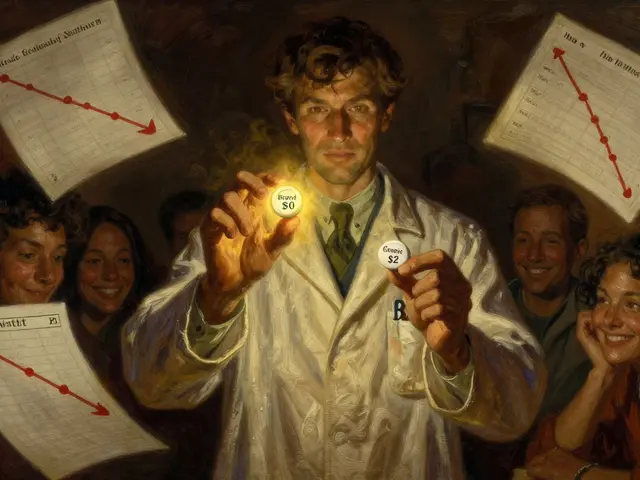
Not all herbs are created equal. Some have real data behind them. Others? Pure guesswork. Ginger is the standout. Multiple studies confirm it reduces nausea and vomiting in early pregnancy, especially at doses under 1,000 mg per day. It’s as effective as some anti-nausea meds, with fewer side effects. The Cleveland Clinic and the American Academy of Family Physicians both say it’s generally safe. Just avoid it if you’re on blood thinners-it can amplify their effects. Raspberry leaf is trickier. Many midwives and birth coaches recommend it in the third trimester to "tone the uterus" and make labor smoother. But here’s what the data says: a 2023 review found women who used it to try to induce labor had a higher chance of needing a C-section. There’s no proof it shortens labor or reduces complications. And because it can stimulate contractions, using it too early could trigger preterm labor. The AAFP classifies it as "likely unsafe" for labor induction. Chamomile is everywhere-tea, capsules, tinctures. People use it for sleep and anxiety. But studies link it to a higher risk of preterm birth, low birth weight, and even a rare heart issue in newborns called ductus arteriosus closure. It’s not banned, but it’s not proven safe either. Cranberry is often taken to prevent urinary tract infections (UTIs), which are common in pregnancy. It might help a little, but it’s not as reliable as antibiotics like nitrofurantoin. Worse, some women report spotting in the second or third trimester after taking cranberry supplements. That’s not normal. Spotting means something’s off-and you need to call your provider. Rosemary is dangerous if taken orally in medicinal amounts. It can stimulate the uterus. Topical use (like in shampoo or lotion) is probably fine, but swallowing rosemary extract? That’s a red flag.The Big Problem: No One’s Asking
Doctors rarely ask about herbal use. Patients rarely volunteer it. Why? Because they assume it’s harmless. Or they’re afraid their provider will judge them. A study in Catalonia found 42% of pregnant women started taking herbal supplements without telling a single healthcare professional. They got advice from their moms, Pinterest, Reddit, or YouTube influencers. One Reddit thread with 142 comments showed 78% of users were unsure if their chosen herb was safe-even though 63% were using one. This silence is dangerous. Imagine you’re taking ginger for nausea and also a prenatal vitamin with iron. No problem. But if you’re also taking a "detox tea" with senna or black cohosh, you’re risking contractions or bleeding. Your OB might never know unless you tell them.
What Experts Actually Say
The American College of Obstetricians and Gynecologists (ACOG) is clear: "Don’t take any herbal product without talking to your provider first." The Cleveland Clinic goes further: "People who are pregnant are encouraged to avoid most herbal supplements." The German Federal Institute for Risk Assessment says women using herbs during pregnancy don’t fit one profile-they’re young, old, educated, not educated. They come from all walks of life. That means every pregnant patient needs to be asked, every time. The FDA’s stance is blunt: "Natural doesn’t mean safe." Two batches of the same herbal product can have wildly different strengths. One might be pure. The next could be laced with toxins. Even traditional knowledge doesn’t guarantee safety. Just because a herb was used for centuries doesn’t mean it’s safe for a developing fetus. Our bodies and pregnancies are different now. We’re older. We’re on more medications. Our diets are different. What worked for your grandmother might not be safe for you.What You Should Do Instead
If you’re thinking about taking an herbal supplement:- Stop. Don’t buy it yet.
- Write down exactly what you’re considering-name, dose, why you want it.
- Call your OB, midwife, or pharmacist. Ask: "Is this safe in pregnancy?" Don’t be embarrassed. They’ve heard it all.
- If they don’t know, ask them to check MotherToBaby.org. It’s a free, science-backed resource updated quarterly.
- Never rely on social media, blogs, or "natural health" influencers.

Why This Matters Beyond Pregnancy
This isn’t just about avoiding a bad outcome. It’s about building trust in healthcare. When women feel judged for using herbs, they stop talking. When providers don’t ask, they miss critical info. That leads to preventable complications. The NIH just launched a $12.7 million study to fill these evidence gaps. But until we have solid data, caution is the only safe choice. And remember: you don’t need to be perfect. You just need to be informed. If you took something before you knew it might be risky, don’t panic. Call your provider. They’re not there to scold you. They’re there to help you move forward safely.What’s Coming Next
Regulators are waking up. In Europe, herbal products must be registered and labeled with pregnancy warnings. The FDA has already issued warning letters to companies making false claims about safety during pregnancy. But the real change will come from conversations. When every pregnant woman feels safe asking, and every provider feels equipped to answer, we’ll start closing the gap. Until then, treat every herbal supplement like a medication-with caution, with questions, and with your provider’s input.Is ginger safe during pregnancy?
Yes, ginger is generally considered safe for nausea in pregnancy when taken at doses under 1,000 mg per day. Multiple studies support its effectiveness and safety for this use. However, avoid it if you’re on blood thinners or have a history of bleeding disorders. Always check with your provider before starting any supplement.
Can raspberry leaf induce labor?
There’s no solid evidence that raspberry leaf induces labor safely. While it’s traditionally used to "tone" the uterus, studies show women who took it to try to start labor had higher rates of C-sections. It can stimulate contractions, so using it before 37 weeks could lead to preterm labor. Most experts recommend avoiding it for labor induction.
Are herbal supplements regulated like drugs?
No. Herbal supplements are classified as dietary supplements, not drugs. That means they don’t need FDA approval for safety or effectiveness before being sold. The FDA can only act after a product is on the market and proven harmful. This leads to inconsistent quality, unlisted ingredients, and unknown risks-especially in pregnancy.
What herbs should I avoid completely during pregnancy?
Avoid pennyroyal, blue cohosh, black cohosh, large amounts of rosemary, and sage. These can stimulate the uterus and increase the risk of miscarriage or preterm labor. Also avoid unregulated "detox" or "cleansing" blends-they often contain hidden laxatives or stimulants. When in doubt, skip it.
Can I take herbal supplements while breastfeeding?
Many herbs pass into breast milk, and safety data is even scarcer than in pregnancy. Ginger and chamomile are often considered low-risk in small amounts, but there’s no guarantee. Always talk to your provider before taking any herb while breastfeeding. What’s safe for you might not be safe for your baby.
Why do so many women use herbal supplements in pregnancy?
Many believe herbal remedies are "natural" and therefore safer than pills. Cultural traditions, family advice, and social media influence play big roles. A Spanish study found women who used herbal products were more likely to believe they should avoid conventional medicine. But "natural" doesn’t mean harmless-especially when the science is missing.
What’s the best way to talk to my doctor about herbal supplements?
Be direct and honest. Say: "I’ve been taking [name of herb] for [reason]. Is this safe?" Bring the bottle or a photo of the label. Don’t wait until you’re in crisis. Ask during your first prenatal visit. Your provider has likely seen this before and wants to help you stay safe.
Are there safer alternatives to herbal supplements for pregnancy symptoms?
Yes. For nausea: ginger (in tea or capsules), vitamin B6, or prescription anti-nausea meds if needed. For sleep: magnesium glycinate, consistent bedtime routines, or prenatal yoga. For UTIs: cranberry juice (not supplements), hydration, and antibiotics like nitrofurantoin if prescribed. For anxiety: therapy, mindfulness, or exercise. These have proven safety data.



Comments(15)