The WHO Model Formulary isn’t a formulary at all - at least not in the way hospitals or insurance companies use the term. It’s a list. A simple, powerful, life-saving list. Created and updated every two years by the World Health Organization, it tells countries what medicines their people actually need to survive. And more than half of those medicines are generics.
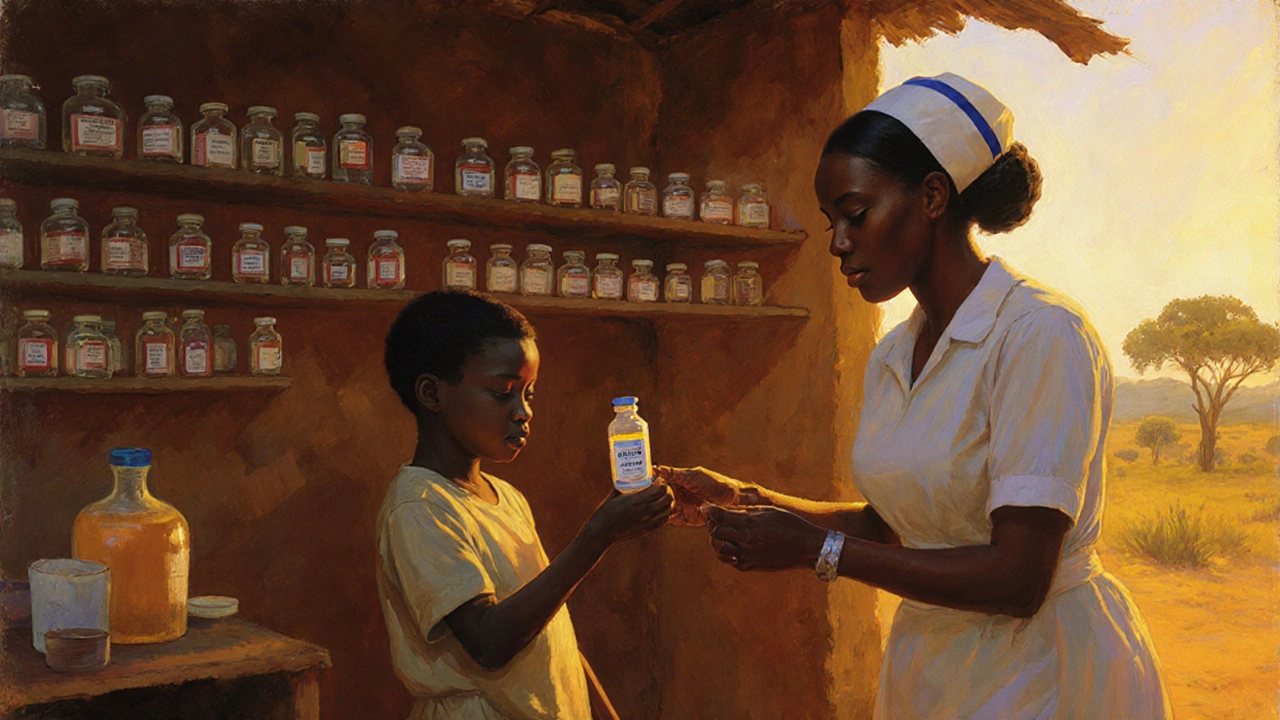
When you hear "essential medicines," think of the basics: antibiotics for pneumonia, insulin for diabetes, antiretrovirals for HIV, blood pressure pills, painkillers, vaccines. These aren’t luxury drugs. They’re the ones you can’t live without. The WHO doesn’t pick them based on profit, marketing, or brand recognition. They’re chosen because they work, they’re safe, and they’re cheap enough for a village clinic in Malawi or a public hospital in Bangladesh to afford.
The 2023 list includes 591 medicines for 369 conditions. Of those, 273 - nearly half - are generic versions. That’s not an accident. It’s the point. Generics make universal health coverage possible. Without them, treating HIV would cost over $1,000 a year per person. With generics? $119. That’s an 89% drop in price since 2008. In 2022, nearly 30 million people living with HIV were on treatment - up from just 800,000 in 2003. That’s the power of the WHO’s focus on affordable generics.
How the WHO Picks What Makes the List
The process isn’t political. It’s scientific. Every two years, 25 independent experts from 18 countries meet in Geneva. They review over 200 requests to add or remove medicines. Each candidate is scored on four things: public health need (30%), proven safety and effectiveness (30%), cost-effectiveness (25%), and whether it can actually be used in real-world clinics (15%). A medicine needs at least a 7.5 out of 10 overall to make the cut.
Evidence matters. The WHO only accepts data from high-quality studies - randomized trials, systematic reviews. No opinion pieces. No sponsored trials without full transparency. In 2023, 94% of inclusions were backed by solid evidence. That’s why some popular drugs in wealthy countries never make the list. If they’re not clearly better than cheaper options, they’re out.
For generics, the bar is even higher. Every single generic on the list must meet WHO Prequalification standards. That means it’s been tested to prove it works just like the original brand - same absorption, same effect. Bioequivalence must be within 80-125% of the brand. For drugs where even a tiny difference can kill - like blood thinners or epilepsy meds - the range tightens to 90-111%.
Core vs. Complementary: What’s Really Essential
The list isn’t one-size-fits-all. It’s split into two parts.
The core list has the bare minimum: medicines that every basic health center should have on hand. Think antibiotics, antimalarials, insulin, birth control pills, asthma inhalers. These are the ones you can give without fancy labs or specialists. They’re meant for primary care - the first point of contact for most people.
The complementary list includes medicines that need more support. Cancer drugs, newer antivirals, biosimilars, treatments requiring lab monitoring. These aren’t less important - they’re just harder to deliver. A rural clinic might not stock them, but a regional hospital should. This split helps countries prioritize. Start with the core. Build up to the rest.
It’s not about having every drug on the shelf. It’s about having the right ones - the ones that save the most lives with the least waste.
Why This List Changes How Countries Spend Money
Over 150 countries have built their own national essential medicines lists based on the WHO model. But here’s the real impact: when countries follow it, they spend less and treat more.
In Ghana, adopting the WHO list led to a 29% drop in out-of-pocket medicine costs between 2018 and 2022. In India, hospitals cut antimicrobial spending by 35% after switching to WHO-recommended generic tiers. Globally, countries using the model saw pharmaceutical costs fall by 23-37% without losing health outcomes.
Why? Because it cuts out the noise. No more paying for expensive brands when a generic does the same job. No more stocking 10 different blood pressure pills because a sales rep visited last month. Just one or two proven, affordable options.
And it’s not just low-income countries. UN agencies like the Global Fund buy 85% of their medicines based on the WHO list. That’s billions of dollars flowing into generic manufacturers who meet quality standards. In 2023, the list directly influenced $15.8 billion in global procurement.

The Generics Gap: Where It Works - and Where It Doesn’t
Having a good list doesn’t mean medicines reach the people who need them.
In Nigeria, a 2022 survey found only 41% of essential medicines were consistently available. Stockouts averaged 58 days per medicine. Why? Not because the list was wrong. Because the supply chain broke. Poor roads, corrupt distributors, delayed payments to suppliers - those are the real killers.
In India, pharmacists report problems with substandard generics slipping into the market. Even if a drug is WHO-prequalified, it can get diluted or fake between the factory and the pharmacy. WHO’s 2022 surveillance found 10.5% of essential medicine samples in low-income countries were substandard or falsified - mostly antibiotics and antimalarials.
And then there’s the industry pushback. In Latin America, generic substitution policies are 32% less effective than in Africa. Why? Strong lobbying from brand-name companies. Doctors used to prescribing the expensive version. Pharmacists paid to push certain brands. Changing habits takes more than a list.
Even in the U.S., where generics dominate the market, the WHO list barely registers. Only 22% of hospital pharmacy directors in the U.S. consult it regularly. Most rely on domestic databases like Micromedex. The WHO list is seen as irrelevant - for "other countries." But that’s changing. As global health threats like antimicrobial resistance grow, U.S. hospitals are starting to look at the WHO’s antibiotic stewardship guidelines.
What’s New in 2023 - And What’s Coming
The 2023 update wasn’t just a tweak. It was a shift.
For the first time, the list included specific rules for biosimilars - cheaper versions of complex biologic drugs like cancer treatments. Seven monoclonal antibodies made the cut, with strict bioequivalence requirements: 85-115% matching the original.
More than 42% of medicines now come in child-friendly forms - dissolvable tablets, flavored syrups, smaller doses. That’s up from 29% in 2019. Kids aren’t small adults. They need medicines that fit their bodies.
The WHO also launched a free app in September 2023. It’s been downloaded over 127,000 times in 158 countries. Nurses in rural clinics use it to check dosing. Pharmacists use it to verify generics. Policymakers use it to justify budget requests.
Looking ahead, the WHO is tying the list tighter to Universal Health Coverage goals. The target? Get essential medicine availability in primary care from 65% today to 80% by 2030. That means more than just listing drugs - it means fixing supply chains, training staff, and funding procurement.
But there’s a catch. Only 31% of low-income countries spend more than 15% of their health budget on medicines - the minimum the WHO says is needed. Without funding, even the best list is just paper.

Is the WHO Model Formulary Flawed?
Yes. But it’s the best we’ve got.
Critics point out that only 12% of new drugs approved between 2018 and 2022 made the 2023 list. High-income countries approved 35-45%. That’s a gap. But the WHO isn’t trying to be the latest-tech list. It’s trying to be the most life-saving list.
Some say the process is too slow. Others worry about industry influence. In 2023, 45% of the evidence used to support inclusions came from industry-funded trials - up from 28% in 2015. The WHO now requires full financial disclosures from experts. All 25 members in 2023 complied.
And yes - it doesn’t solve everything. It doesn’t fix broken supply chains. It doesn’t pay for nurses. It doesn’t stop counterfeit drugs. But it gives countries a roadmap. A science-based, affordable, equitable blueprint.
Without it, the world would be drowning in expensive, unproven, over-marketed drugs - and millions would still die from pneumonia, diabetes, or HIV because the medicine they needed was too expensive to find.
What You Can Do With This Information
If you’re a policymaker: Use the WHO list to build your national essential medicines list. Start with the core. Prioritize generics. Demand WHO Prequalification.
If you’re a pharmacist: Push for generic substitution where it’s safe. Train staff on bioequivalence. Report substandard drugs.
If you’re a patient or advocate: Ask your clinic: "Do you stock WHO-recommended generics?" If not, why not? Demand transparency.
If you’re in global health: Fund the supply chains. Support local generic manufacturers. Don’t just fund drugs - fund the system that delivers them.
The WHO Model Formulary isn’t magic. But it’s the closest thing we have to a global health justice tool. It says: Your life matters, no matter where you live. And the medicine you need shouldn’t cost more than your rent.
Is the WHO Model Formulary a legal requirement for countries?
No. The WHO Model List is a recommendation, not a law. But over 150 countries use it as the foundation for their own national essential medicines lists. It’s the most trusted global standard because it’s based on evidence, not politics. Countries that follow it see better health outcomes and lower costs.
Are all generics on the WHO list the same quality?
Yes - if they’re on the list. Every generic included must meet WHO Prequalification standards, meaning it’s been independently tested to prove it works just like the original brand. This includes strict bioequivalence tests. But once it leaves the factory, quality can drop. Substandard or fake medicines still enter supply chains in some countries, especially for antibiotics and antimalarials.
Why doesn’t the WHO list include every new drug?
Because the WHO doesn’t prioritize novelty - it prioritizes need. A brand-new cancer drug might cost $100,000 a year. If there’s a cheaper, proven alternative that works for 80% of patients, the WHO picks the alternative. The goal is to save the most lives with limited resources, not to offer the latest science.
Can low-income countries actually afford to follow the WHO list?
They can - if they prioritize. The list is designed to be affordable. But funding is the real barrier. Only 31% of low-income countries spend enough on medicines to make the list work. The problem isn’t the drugs - it’s the system. Without reliable supply chains, trained staff, and dedicated budgets, even the best list won’t help.
How does the WHO Model List compare to U.S. insurance formularies?
They’re designed for completely different goals. U.S. insurance formularies are built to control costs for private payers - they use tiers, copays, and step therapy to steer patients toward cheaper drugs. The WHO list doesn’t care about patient copays. It cares about whether a medicine saves lives in a clinic with no electricity. It picks one best option per condition, not two or three. It’s about public health, not profit.



Comments(14)