Most people think of overdose as something that happens to someone else-until it doesn’t. A missed dose, a mix-up with pills, or even just taking one extra tablet can turn dangerous fast. The good news? For many common drug overdoses, there’s a specific antidote that can save a life-if it’s given in time. This guide cuts through the noise and tells you exactly what antidotes exist, how they work, when they matter, and what you need to do if you or someone you care about is in trouble.
Acetaminophen Overdose: The Silent Killer
Acetaminophen (known as paracetamol outside the U.S.) is in over 600 medications-from pain relievers to cold and flu combos. It’s safe at normal doses. But take more than 10 grams in a single day, or just a few extra pills over 24 hours, and your liver starts to die. The scary part? You might feel fine for hours, even a full day. No vomiting. No pain. Just quiet, invisible damage.
The antidote is N-acetylcysteine, or NAC. It works by replacing the liver’s depleted supply of glutathione, the molecule that neutralizes the toxic byproduct of acetaminophen breakdown. Timing is everything. If NAC is started within 8 hours of ingestion, it’s 98% effective at preventing liver failure. After 16 hours, the chances of survival drop sharply.
How it’s given: In the hospital, it’s an IV drip over 21 hours. Oral NAC tastes awful-like rotten eggs-but it’s just as effective if you can keep it down. The full dose is 133 grams. Hospitals stock it because it’s cheap, safe, and life-saving. Don’t wait for symptoms. If you suspect an overdose, go to the ER immediately-even if you feel fine. The Rumack-Matthew nomogram, a chart doctors use, helps decide if you need it based on your blood level and time since ingestion.
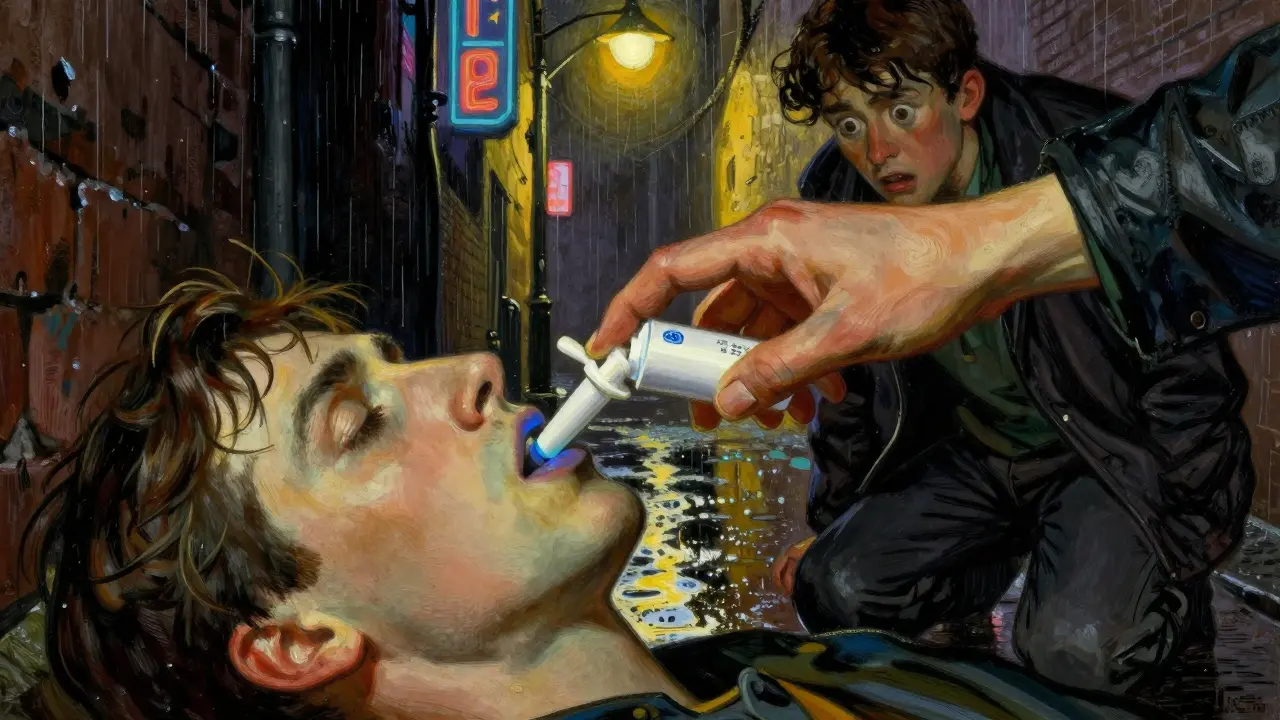
Opioid Overdose: Naloxone Can Bring Someone Back
Opioids-prescription painkillers like oxycodone, illegal drugs like heroin, or even fentanyl-are the leading cause of overdose deaths in the U.S. and New Zealand. The problem? They slow or stop breathing. Without oxygen, brain damage happens in minutes.
Naloxone is the antidote. It kicks opioids off the brain’s receptors and reverses the overdose in 2 to 5 minutes. It’s not a cure-it’s a bridge. Its effects last only 30 to 90 minutes. If the opioid was long-acting (like methadone), the person can slip back into overdose after naloxone wears off. That’s why calling emergency services is non-negotiable.
How to use it: Naloxone comes as a nasal spray (like Narcan or Kloxxado) or an auto-injector. One spray into one nostril is enough to start. If there’s no response in 3 minutes, give a second dose. You can’t overdose on naloxone. It won’t hurt someone who hasn’t taken opioids. Since March 2023, the FDA approved Narcan for over-the-counter sale. It’s now available at pharmacies without a prescription in most places.
Real story: In Victoria, Australia, over 25,000 naloxone kits have been given out since 2017. There have been 1,842 documented reversals. One nurse on Reddit described giving naloxone to a young man who woke up angry and combative. That’s normal. The sudden reversal can cause withdrawal-shaking, nausea, panic. Stay calm. Keep him on his side. Wait for EMS.
Benzodiazepine Overdose: When Calm Turns Dangerous
Benzodiazepines-like Xanax, Valium, or Klonopin-are prescribed for anxiety, insomnia, and seizures. They’re safe when taken as directed. But mixing them with alcohol or opioids is deadly. They can cause deep sedation, slow breathing, and coma.
The antidote is flumazenil. It works by blocking benzodiazepines from binding to brain receptors. But here’s the catch: it’s risky. If someone has been taking benzodiazepines daily for months or years, flumazenil can trigger violent seizures. That’s why doctors avoid it unless it’s a clear, isolated overdose.
How it’s given: A tiny IV dose of 0.2 mg, then 0.3 mg every minute up to 3 mg total. Too fast, and the patient can wake up terrified, confused, or even aggressive. Many ERs now prefer supportive care-oxygen, breathing support, monitoring-instead of flumazenil. The California Poison Control System warns: “Use with caution in patients on chronic benzodiazepine therapy.”
If you or someone you know takes benzodiazepines daily, never mix them with alcohol or opioids. Keep the prescription bottle handy. If an overdose is suspected, call emergency services and place the person on their side. Don’t try to make them vomit. Don’t give them coffee. Just wait for help.
Toxic Alcohol Poisoning: Methanol and Ethylene Glycol
These aren’t your typical drugs. Ethylene glycol is in antifreeze. Methanol is in windshield washer fluid, some hand sanitizers, and homemade alcohol. Ingesting even a small amount can cause blindness, organ failure, or death.
The antidote is fomepizole. It blocks the enzyme that turns these poisons into deadly acids in the body. The standard dose is 15 mg/kg IV, then 10 mg/kg every 12 hours. It’s expensive-up to $4,000 per treatment-but it’s safer and easier to use than the old alternative: ethanol (vodka or whiskey). Yes, you read that right. In emergencies, some hospitals use high-proof alcohol as a temporary fix because fomepizole isn’t available.
Why it matters: Symptoms start with nausea and dizziness, then progress to confusion, seizures, and coma. By the time someone looks really sick, it’s often too late. If you suspect someone drank antifreeze or a suspicious homemade drink, get them to the hospital immediately. Blood tests will show the toxin levels. Time is measured in hours, not days.
Methemoglobinemia: When Blood Can’t Carry Oxygen
This rare condition happens when certain drugs-like benzocaine (in numbing sprays), dapsone (an antibiotic), or nitrites (poppers)-turn hemoglobin into methemoglobin, which can’t carry oxygen. Skin turns blue. Breathing gets hard. People feel like they’re suffocating, even with plenty of air.
The antidote is methylene blue. It’s given as an IV push over 5 minutes. The dose is 1 to 2 mg per kg of body weight. Don’t exceed 7 mg/kg total. It works fast-often within minutes. But it’s not for everyone. People with G6PD deficiency (a genetic condition) can have dangerous reactions. That’s why doctors test before giving it.
If someone turns blue after using a numbing spray or snorting poppers, call 911. Don’t wait. Oxygen and methylene blue can reverse this in minutes. But without treatment, it can be fatal.
What You Can Do Right Now
You don’t need to be a doctor to be prepared. Here’s what you can do today:
- Keep naloxone nasal spray at home if you or someone you live with takes opioids-even if they’re prescribed. It’s available without a prescription in most pharmacies.
- Store all medications in locked cabinets. Kids and teens are at risk of accidental overdose.
- Never mix alcohol with painkillers, sleep aids, or anxiety meds. That’s how most overdoses happen.
- Know the signs: Unresponsiveness, slow or shallow breathing, blue lips, pinpoint pupils, extreme drowsiness.
- Save your local poison control number. In New Zealand, it’s 0800 764 766. In the U.S., it’s 1-800-222-1222. They’re staffed 24/7 by toxicology experts.

Myths That Can Kill
Myth: “If they’re breathing, they’re fine.”
Truth: Opioid overdoses can cause breathing to slow so much it’s almost undetectable. If someone’s barely breathing, they’re in cardiac arrest mode.
Myth: “I’ll just wait and see if they get worse.”
Truth: With acetaminophen, you have an 8-hour window. After that, the damage is done. No second chances.
Myth: “Naloxone is only for drug addicts.”
Truth: Naloxone saves the lives of people who took a prescription too high, mixed meds with alcohol, or were given the wrong dose in a hospital. It doesn’t care who you are.
Myth: “Home remedies work-coffee, cold showers, vomiting.”
Truth: None of these reverse an overdose. They waste time. Call for help. Use naloxone if you have it. Put them on their side. Wait.
When to Call Emergency Services
Call immediately if someone has:
- Stopped breathing or is breathing less than 8 times per minute
- Is unconscious or can’t be woken up
- Has blue or gray lips or fingernails
- Has pinpoint pupils
- Is vomiting and unresponsive
Even if you’re not sure-call. Poison control centers handle over 2 million cases a year in the U.S. alone. Most are managed without hospital visits. But if there’s any doubt, treat it like a medical emergency. Your quick action could mean the difference between life and death.
What Hospitals Do When You Arrive
Don’t panic if you get to the ER and they ask a lot of questions. They need to know:
- What drug was taken?
- How much?
- When?
- Was it mixed with anything?
- Does the person have other health problems?
They’ll check vital signs, run blood tests, and give the right antidote-sometimes before you finish answering. NAC, naloxone, and methylene blue are all kept on hand in most emergency departments. Fomepizole might take a little longer to get, but they’ll start treatment with ethanol if needed.
The goal isn’t just to reverse the overdose. It’s to prevent long-term damage. That’s why you might stay overnight-even if you feel fine after naloxone.
Can I keep naloxone at home?
Yes. Naloxone nasal spray is now available over the counter at most pharmacies without a prescription. It’s safe, easy to use, and can reverse an opioid overdose in minutes. Keep one in your bag, car, or home if you or someone you live with uses opioids-even if they’re prescribed. Training is minimal: one spray into one nostril. No needles. No training needed.
Is NAC available without a prescription?
No. N-acetylcysteine (NAC) is only available by prescription or in hospital settings. It’s not sold as an over-the-counter antidote. If you suspect an acetaminophen overdose, go to the ER immediately. Do not wait. Don’t try to buy NAC online or use supplements-they’re not the same thing and won’t work.
Can I use alcohol as an antidote for antifreeze poisoning?
In extreme emergencies, when fomepizole isn’t available, some hospitals use high-proof ethanol (vodka or whiskey) to slow down the metabolism of methanol or ethylene glycol. But this is only done under strict medical supervision. Do not try this at home. Drinking alcohol won’t help and can make things worse. Call emergency services immediately if you suspect toxic alcohol ingestion.
Do antidotes work for all types of overdoses?
No. There are only a handful of specific antidotes-for acetaminophen, opioids, benzodiazepines, toxic alcohols, methemoglobinemia, and a few others. Most overdoses, especially from antidepressants, stimulants, or herbal supplements, don’t have antidotes. Treatment is supportive: breathing support, IV fluids, heart monitoring. That’s why calling emergency services is always the first step.
What if I give naloxone and the person doesn’t wake up?
Give a second dose after 3 minutes. If there’s still no response, continue CPR and wait for emergency responders. Naloxone only works on opioids. If the overdose was caused by something else-like alcohol, benzodiazepines, or cocaine-naloxone won’t help. But giving it won’t hurt. Always call for help, even if you think you did everything right.






Comments(15)