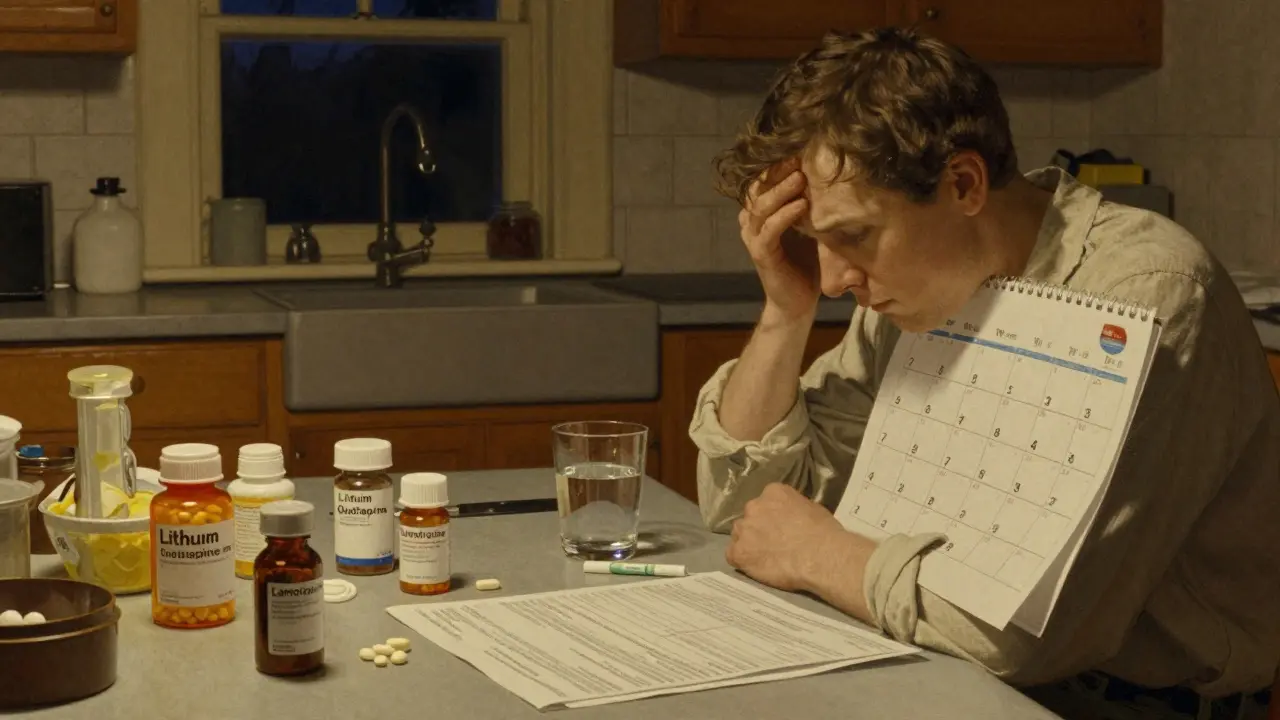
Managing bipolar disorder isn’t about finding one magic pill-it’s about finding the right balance.
If you or someone you know has bipolar disorder, you’ve probably heard the same advice: medication is essential. But what does that actually mean day to day? It’s not just taking a pill and hoping for the best. It’s tracking blood levels, dealing with weight gain, fighting brain fog, and sometimes switching meds three times before finding something that doesn’t leave you feeling like a zombie. And yet, for many, it’s the difference between surviving and thriving.
Let’s cut through the noise. This isn’t a textbook overview. This is what actually happens when lithium, quetiapine, lamotrigine, or other meds are used in real life-with all the wins, the setbacks, and the hard choices.
Lithium: The OG Mood Stabilizer That Still Works
Lithium has been around since the 1970s. It’s old, cheap, and still the gold standard for long-term stability. Studies show it cuts suicide risk by 80% compared to no treatment. That’s not a small number. It’s life-saving.
But here’s the catch: you have to monitor it like a hawk. Blood levels need to stay between 0.6 and 1.0 mmol/L. Too low? You’re back to mood swings. Too high? You’re at risk for tremors, confusion, even seizures. That’s why blood tests are weekly at first, then every 2-3 months once you’re stable.
Side effects? Almost everyone gets them. Constant thirst. Urinating every hour. Hand tremors so bad you can’t hold a coffee cup. Weight gain of 10-15 pounds in the first year. Nausea. These aren’t rare. They’re expected. One Reddit user said they drank 3 liters of water a day and still felt dehydrated. That’s lithium.
And yet, people stay on it. Why? Because when it works, it works deeply. One user with 85 upvotes on r/Bipolar wrote: “I gained 15 pounds, but it’s worth not having suicidal depression every week.” That’s the trade-off. And for many, it’s worth it.
Antipsychotics: Faster Relief, Heavier Costs
Quetiapine (Seroquel), olanzapine, risperidone, aripiprazole-these are the antipsychotics now commonly used for bipolar disorder. Unlike lithium, they don’t need blood tests. That’s a relief for some. But they bring their own problems.
Quetiapine works fast. People report feeling better in as little as 7 days. That’s why it’s often used in acute episodes. But it’s also notorious for weight gain. Studies show users gain an average of 4.6kg in just 6 weeks. On PatientsLikeMe, 68% reported gaining 22 pounds on average. That’s not just cosmetic-it increases diabetes risk by 20-30% with olanzapine.
Sedation is another big one. Sixty to seventy percent of people on quetiapine feel drowsy. Some use it as a sleep aid. Others can’t get through the workday. Akathisia-restlessness you can’t shake-hits 15-20% of users. It feels like your nerves are buzzing under your skin.
But here’s the upside: they’re effective for mania. Risperidone hits a 68% response rate in 3 weeks. That’s better than lithium for acute episodes. And newer ones like lumateperone (Caplyta) are coming in with minimal weight gain-just 0.8kg in 6 weeks, compared to 3.5kg for quetiapine. That’s a game-changer for people tired of the scale.
Lamotrigine: The Depression Specialist With a Hidden Risk
If your main struggle is depression-not mania-lamotrigine might be your best bet. It’s the only mood stabilizer proven to help bipolar depression without triggering mania. Response rates? 47% vs. 28% for placebo. And it doesn’t cause weight gain. That’s huge.
But here’s the catch: it has to be started slowly. Too fast, and you risk a rare but deadly skin rash called Stevens-Johnson syndrome. The risk is about 1 in 1,000, but it’s real. Doctors start at 25mg once a week, then slowly increase over months. Patience is required.
Some users report insomnia on lamotrigine. Others say it’s the only thing that lifted their fog without making them gain weight. One person on Reddit said: “I switched from lithium to lamotrigine. The thirst stopped. But now I can’t sleep. I’m choosing sleep over stability.” That’s the kind of hard call people face every day.

Combination Therapy: When One Drug Isn’t Enough
Many people don’t respond to one medication alone. That’s when doctors add a second. A mood stabilizer plus an antipsychotic. This combo works for about 70% of treatment-resistant cases.
But it’s not without cost. Side effects pile up. Weight gain. Sedation. Metabolic issues. One study showed side effect burden increases by 25-30% with combination therapy. That’s why it’s not the first move. It’s the second-or third.
Long-acting injectables like Abilify Maintena (monthly shots of aripiprazole) are changing the game for people who forget pills. No more daily routines. No more missed doses. Just one shot a month. But the side effects? Still there. And you can’t stop it once it’s in your system.
What About Antidepressants?
Here’s where things get controversial. Antidepressants like fluoxetine (Prozac) can help with bipolar depression. But they carry a 10-15% risk of flipping you into mania. Some experts say never use them. Others say use them cautiously-with a mood stabilizer in place.
Dr. Gary Sachs from Harvard warns that 25% of people on antidepressants alone switch into mania. Dr. David Miklowitz at UCLA says, “If the depression is severe and the person is stable, it’s okay to try.” There’s no universal answer. It depends on your history, your triggers, your tolerance for risk.
Most psychiatrists now avoid antidepressants unless absolutely necessary. And even then, they’re paired with a mood stabilizer. Always.
Monitoring: The Unspoken Part of Treatment
Medication isn’t a set-it-and-forget-it deal. You need to track more than just mood.
Every three months, you should get checked for:
- Weight and waist circumference (over 40 inches for men, 35 for women = metabolic risk)
- Fasting blood sugar and cholesterol
- Thyroid and kidney function (especially if on lithium)
These aren’t optional. They’re part of the treatment plan. Olanzapine can send your blood sugar soaring. Lithium can damage your kidneys over time. Catching it early means you can switch meds or add metformin to help.
And drug interactions? Big risk. NSAIDs like ibuprofen can spike lithium levels into toxic range. Even a single dose of Advil can be dangerous. Antipsychotics interact with over 40 common meds-antibiotics, heart pills, even some herbal supplements. Always tell every doctor you see: “I’m on bipolar meds.”
Why People Quit-and What Helps Them Stay
Forty percent of people stop their meds within a year. Why? Side effects. A NAMI survey of 1,200 people found:
- 78% quit because of weight gain
- 65% said they felt mentally foggy
- 52% struggled with sexual dysfunction
But here’s the thing: quitting doesn’t mean you failed. It means the plan didn’t fit. The goal isn’t to stay on a drug you hate. It’s to find one you can live with.
People who stick with treatment often do so because they have:
- A psychiatrist who listens
- A plan for side effects (like metformin for weight gain)
- Support from others who get it
One user’s tip: “Take lithium with food. Split the dose. Drink water slowly, not all at once.” Small tricks make a big difference.
The Future: Personalized Treatment Is Here
Genetic testing is starting to help. Companies like Genomind test for CYP2D6 and CYP2C19 gene variants-genes that affect how your body processes 40% of bipolar meds. If you’re a slow metabolizer, standard doses can make you sick. If you’re fast, you need more. Testing can cut trial-and-error time by 30%.
New drugs are coming. Lumateperone (Caplyta) works for depression with almost no weight gain. Cariprazine and lurasidone are now first-line for bipolar depression in the latest guidelines. Digital tools like reSET-BD, an app that tracks mood and medication adherence, reduced relapse by 22% in trials.
By 2027, experts predict personalized treatment will be standard-not a luxury. But for now, it’s still a mix of science, patience, and persistence.
Final Thought: It’s Not Perfect, But It’s Possible
Bipolar disorder treatment isn’t about being cured. It’s about managing. About finding the version of yourself that can show up for work, for family, for life-even if you’re on meds that make you tired, thirsty, or heavier than you want to be.
There’s no perfect drug. But there are good enough ones. And sometimes, that’s all you need.
Can you take lithium and antipsychotics together?
Yes, combining lithium with an antipsychotic like quetiapine or aripiprazole is common-especially for treatment-resistant cases. About 70% of people who don’t respond to one drug alone improve with this combo. But side effects like weight gain, drowsiness, and metabolic issues increase by 25-30%. Blood levels of lithium must still be monitored closely, as antipsychotics don’t interfere with lithium testing but can worsen its side effects.
How long does it take for mood stabilizers to work?
Lithium and valproate usually take 1-3 weeks to show full effect for mania, and 4-6 weeks for depression. Lamotrigine is slower-it can take 2-3 months to reach full benefit for depression, which is why dosing starts so low. Antipsychotics like quetiapine work faster, often showing improvement in 7 days. The key is patience and consistency. Don’t quit before giving it time.
Is there a bipolar medication with no side effects?
No. All medications for bipolar disorder come with side effects. Even newer drugs like lumateperone (Caplyta), which has minimal weight gain, can still cause dizziness, nausea, or fatigue. The goal isn’t to find a drug with no side effects-it’s to find the one where the benefits outweigh the downsides. For some, weight gain is worth stopping weekly suicidal thoughts. For others, brain fog is too high a price for mood stability.
Can you stop bipolar meds if you feel fine?
Stopping meds without medical supervision is one of the biggest risks for relapse. Even if you feel stable, your brain chemistry may still need support. Studies show over 70% of people who quit their meds relapse within a year. If you want to stop, work with your doctor to taper slowly-over months, not days. Never stop cold turkey.
What’s the cheapest effective treatment for bipolar disorder?
Lithium carbonate is the most cost-effective option. Generic lithium costs $4 to $40 a month, depending on your pharmacy and insurance. In contrast, brand-name antipsychotics like Vraylar can cost over $1,200 a month. Even though lithium requires regular blood tests, the overall cost is far lower. Many people use lithium as a long-term foundation and add cheaper generics like lamotrigine ($15-$50/month) for depression support.



Comments(15)