C. difficile colitis isn’t just a bad case of diarrhea. It’s a dangerous infection that can turn deadly - especially when antibiotics, meant to help, end up making things worse. Every year in the U.S., about half a million people get infected with Clostridioides difficile, and nearly 30,000 die from it. The real kicker? Most of these cases start because someone took an antibiotic. Not the wrong one - any one.
How Antibiotics Set Off a C. diff Explosion
Your gut is home to trillions of bacteria. Most of them are harmless, some are helpful. They keep bad actors like C. difficile in check. But when you take antibiotics, especially broad-spectrum ones, you don’t just kill the bad bacteria. You wipe out the good ones too. That’s when C. difficile gets its chance.It’s not that antibiotics cause C. difficile. The bacteria are already out there - in hospitals, nursing homes, even in your own gut. But without the normal gut flora to hold it back, it multiplies fast and starts producing toxins that rip apart the colon lining. That’s when diarrhea, fever, and abdominal pain show up. In severe cases, it leads to toxic megacolon, colon rupture, or sepsis.
Some antibiotics are way more dangerous than others. A 2023 study tracking over 33,000 hospital stays found that piperacillin-tazobactam - a common IV antibiotic - had the highest risk, nearly doubling the chance of C. diff infection. Other high-risk drugs include clindamycin, later-generation cephalosporins like ceftriaxone, and carbapenems. Even fluoroquinolones like ciprofloxacin, once considered safe, now carry a strong warning.
On the flip side, tetracyclines like doxycycline show much lower risk. That doesn’t mean they’re harmless, but they’re less likely to wipe out your gut flora completely. The key takeaway? The longer you’re on antibiotics - especially beyond 14 days - the higher your risk. Each extra day increases the chance of infection by 8%.
Why Stopping the Antibiotic Isn’t Always Enough
You’d think if you stop the antibiotic that caused the problem, your body would bounce back. And sometimes, it does. The Cleveland Clinic says for some people, just stopping the drug is enough. Their immune system and remaining good bacteria clean up the mess.But for others, it’s not that simple. Once C. difficile takes hold, it forms spores that survive in your gut for weeks. Even after symptoms go away, those spores can wake up again. That’s why recurrence is so common - about 20% of people get it again after their first infection. And if you’ve had one recurrence, your chance of another jumps to 40-60%.
Doctors often prescribe vancomycin or fidaxomicin to treat the infection. Vancomycin works, but it’s not great at preventing relapse. Fidaxomicin is better - it targets C. difficile more precisely and leaves other gut bacteria alone. Still, even with fidaxomicin, about 1 in 5 people end up back in the hospital with another flare-up.
And here’s the scary part: if you’re already carrying C. difficile without symptoms - which happens in up to 5% of healthy adults - antibiotics can trigger an infection almost immediately. One study showed asymptomatic carriers had a 27 times higher risk of developing full-blown colitis after taking antibiotics. That’s why just avoiding antibiotics isn’t enough. You need to avoid unnecessary ones altogether.
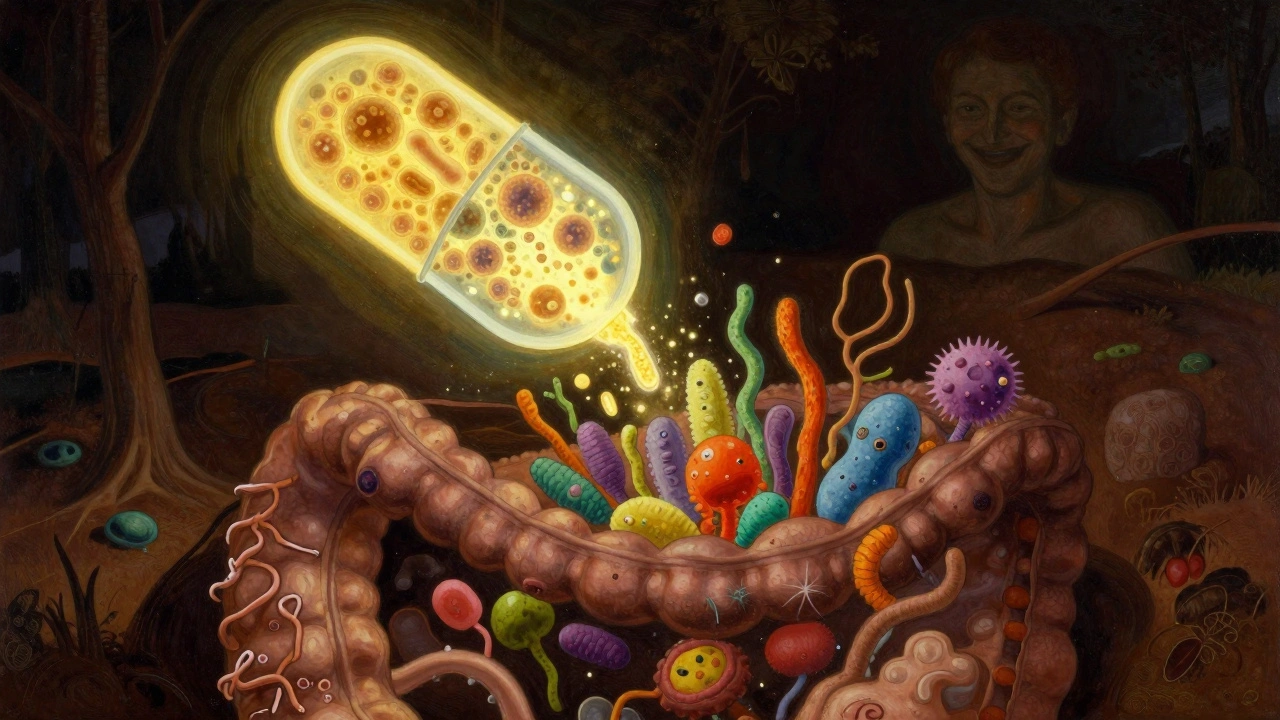
What Is a Fecal Transplant - and Why Does It Work?
Fecal microbiota transplantation (FMT) sounds gross. And yeah, it involves taking stool from a healthy donor and putting it into the colon of someone with recurrent C. diff. But it’s not magic. It’s science.Think of your gut like a garden. Antibiotics kill off the good plants. C. difficile is the weed that takes over. FMT doesn’t kill the weed. It replants the whole garden with healthy soil - meaning, a diverse mix of good bacteria from a donor’s stool.
The first big proof came in 2013, in a landmark study published in the New England Journal of Medicine. Researchers compared FMT to standard vancomycin treatment for people with multiple recurrences. The results were shocking: 94% of FMT patients were cured after one or two treatments. Only 31% of those on vancomycin were.
Since then, dozens of studies have confirmed it. The American Gastroenterological Association now recommends FMT for anyone who’s had three or more C. diff infections. Success rates? Between 85% and 90%. That’s better than any drug.
How it’s done has evolved. Originally, it was done via colonoscopy - the donor stool was delivered directly into the colon. Now, many patients get it as a capsule you swallow. There’s also enema delivery. The capsules are easier, less invasive, and just as effective. One approved product, Rebyota, is now sold as a standardized, FDA-approved treatment - not just a doctor-prepared mixture.

Why FMT Beats Antibiotics for Recurrent Cases
Antibiotics treat the infection, but they don’t fix the broken ecosystem. That’s why they fail over and over. FMT fixes the root cause: the lack of healthy bacteria.After FMT, the donor’s microbes quickly colonize the gut. They outcompete C. difficile for space and nutrients. They also produce substances that directly suppress the pathogen. In some cases, the patient’s gut microbiome looks almost identical to the donor’s within days.
It’s not just about stopping diarrhea. People who’ve had multiple recurrences often describe life before FMT as a nightmare - constant bathroom trips, fear of leaving home, weight loss, depression. One Reddit user wrote: “I had five relapses. Vancomycin helped for a while, then it came back worse. FMT? I haven’t had a single symptom since.”
And it’s cost-effective. A single FMT procedure costs $1,500 to $3,000. A hospital stay for a recurrent C. diff infection? Around $11,000. Multiply that by five recurrences - and you’re looking at $55,000 in medical bills. FMT saves money and lives.
What About Probiotics? Are They a Good Alternative?
You’ve probably heard that probiotics can help with gut health. So why not just take a pill instead of a fecal transplant?The short answer: no. Not for C. diff.
The Infectious Diseases Society of America reviewed dozens of studies and concluded there’s insufficient evidence to recommend probiotics for preventing or treating C. diff. Some products may even be dangerous - especially for people with weakened immune systems. There have been cases of probiotic strains causing bloodstream infections.
Even kefir, a fermented milk drink sometimes touted as a natural remedy, hasn’t held up in rigorous trials. One small study suggested it might help when combined with tapering antibiotics, but it’s not reliable. And it’s nowhere near as effective as FMT.
Probiotics are not a substitute. They’re not even a backup plan. For recurrent C. diff, FMT is the only proven solution.
The Future: Beyond the Poop
FMT works, but it’s not perfect. Donor screening is strict - but not foolproof. There’s still a small risk of transferring other pathogens. That’s why the FDA is pushing for standardized products.Two FDA-approved microbiome therapies hit the market in 2022 and 2023: Rebyota and Vowst. These aren’t raw stool. They’re purified, frozen, capsule-form collections of specific bacterial strains selected for their ability to fight C. diff.
Even more promising is SER-109, an oral microbiome therapeutic tested in a Phase 3 trial called PUNCH CD3. It had an 88% cure rate - almost as good as FMT - without any fecal matter. It’s made from purified bacterial spores, so it’s clean, shelf-stable, and easy to take.
These aren’t just alternatives. They’re the future. No more “yuck factor.” No need for donor matching. Just a pill you swallow.
What You Can Do Right Now
If you’re on antibiotics:- Ask your doctor: “Is this antibiotic really necessary?”
- Ask: “Can we use a narrower-spectrum drug instead?”
- Ask: “How long do I really need to take this?”
Don’t assume antibiotics are harmless. Even a 5-day course of amoxicillin can increase your C. diff risk. The CDC’s “Start Smart - Then Focus” program says: review all antibiotic prescriptions within 48 to 72 hours. If you’re not getting better, stop and reassess.
If you’ve had C. diff before:
- Avoid antibiotics unless absolutely necessary.
- Know the signs of recurrence: watery diarrhea, fever, cramps, loss of appetite.
- If you’ve had two or more recurrences, talk to a gastroenterologist about FMT.
It’s not about fear. It’s about awareness. Antibiotics save lives - but they can also start a chain reaction that ends in disaster. FMT doesn’t just treat C. diff. It restores your body’s natural balance. And sometimes, that’s the only thing that works.
Can C. diff go away on its own without treatment?
In mild cases, especially in younger, healthy people, C. diff can resolve on its own after stopping the triggering antibiotic. The body’s natural immune response and remaining gut bacteria may clear the infection. But this isn’t reliable. For older adults, those with weakened immune systems, or anyone with severe symptoms like high fever or bloody diarrhea, untreated C. diff can quickly turn deadly. Never assume it will go away - always get it checked.
Is fecal transplant safe? What are the risks?
FMT is considered very safe when done through approved methods and screened donors. The biggest risks are short-term: bloating, cramping, or temporary diarrhea. Long-term risks are rare but real - including possible transfer of antibiotic-resistant bacteria, viruses, or even unknown pathogens. That’s why FDA-approved products like Rebyota and Vowst are preferred over donor stool from unregulated sources. People with compromised immune systems should be especially cautious. But for recurrent C. diff, the benefits far outweigh the risks.
Why isn’t FMT used as a first-line treatment?
FMT is not used first because most people with their first C. diff infection respond well to antibiotics like vancomycin or fidaxomicin. FMT is reserved for recurrent cases because it’s more invasive, requires donor screening, and isn’t needed for simple cases. Guidelines recommend it only after two or three recurrences. But as standardized products become easier to use and more affordable, that may change.
Can you get C. diff from food or water?
C. diff spores are found in soil, water, and animal feces, but you don’t typically get infected from food or water. The main transmission route is person-to-person, especially in healthcare settings. Spores stick to surfaces - doorknobs, bedrails, phones - and are spread by hands that aren’t washed properly. That’s why handwashing with soap and water (not just hand sanitizer) is critical in hospitals and homes with infected people.
Are there any new drugs coming to replace FMT?
Yes. Two FDA-approved microbiome therapies - Rebyota and Vowst - are already on the market. More are in development, like SER-109, which uses purified bacterial spores in pill form. These are designed to be as effective as FMT but without the stool. They’re easier to store, transport, and administer. In the next 5 years, these products could become the standard for recurrent C. diff, replacing traditional FMT in most clinics.






Comments(11)