Chronic tension headaches aren’t just bad days. They’re a daily grind-like a tight band wrapped around your skull, 15 or more days a month, for three months straight. If you’ve been told it’s just stress, or that you’re overreacting, you’re not alone. Most people with this condition wait over two years before getting the right diagnosis. And here’s the truth: it’s not your muscles tightening up. It’s your brain becoming too sensitive to pain. That’s the modern science. The old idea of muscle tension causing these headaches? It’s outdated, but still widely repeated-even by some doctors.
What Exactly Is a Chronic Tension Headache?
By the official medical standard (ICHD-3), chronic tension headache means you have headaches on 15 or more days each month for at least three months. And on at least eight of those days, the pain must match the classic tension-type pattern: dull, pressing, not throbbing, and felt on both sides of your head. No nausea, no vomiting, no light or sound sensitivity-those are migraine signs. If you have those, it’s probably not tension headache.
The pain isn’t severe. Most people rate it around 5 out of 10. But it doesn’t go away. It lingers. You might feel it in your temples, the back of your neck, or across your forehead. And if your doctor presses on your scalp or neck muscles, they’ll likely find tenderness-especially in the temporalis, trapezius, or suboccipital areas. That doesn’t mean those muscles are the cause. It means your brain is amplifying the signals from them.
What makes this different from episodic tension headaches? Frequency. Episodic happens less than 15 days a month. Chronic is daily life. And here’s the kicker: about 3.4% of people with episodic tension headaches turn chronic each year. It creeps up. You don’t wake up one day with it. You slowly start needing painkillers more often, sleeping worse, feeling more stressed-and then the headaches start sticking around.
What’s Really Causing It? (Spoiler: It’s Not Stress Alone)
Stress is the usual suspect. And yes, 89% of people with chronic tension headaches say stress makes it worse. But here’s what the data doesn’t tell you: most headaches don’t happen during the stressful moment. They happen after. When your body tries to relax. When you finally stop working. When you lie down. That’s when cortisol drops, your nervous system shifts, and your brain misfires. It’s not the stress itself-it’s the crash after.
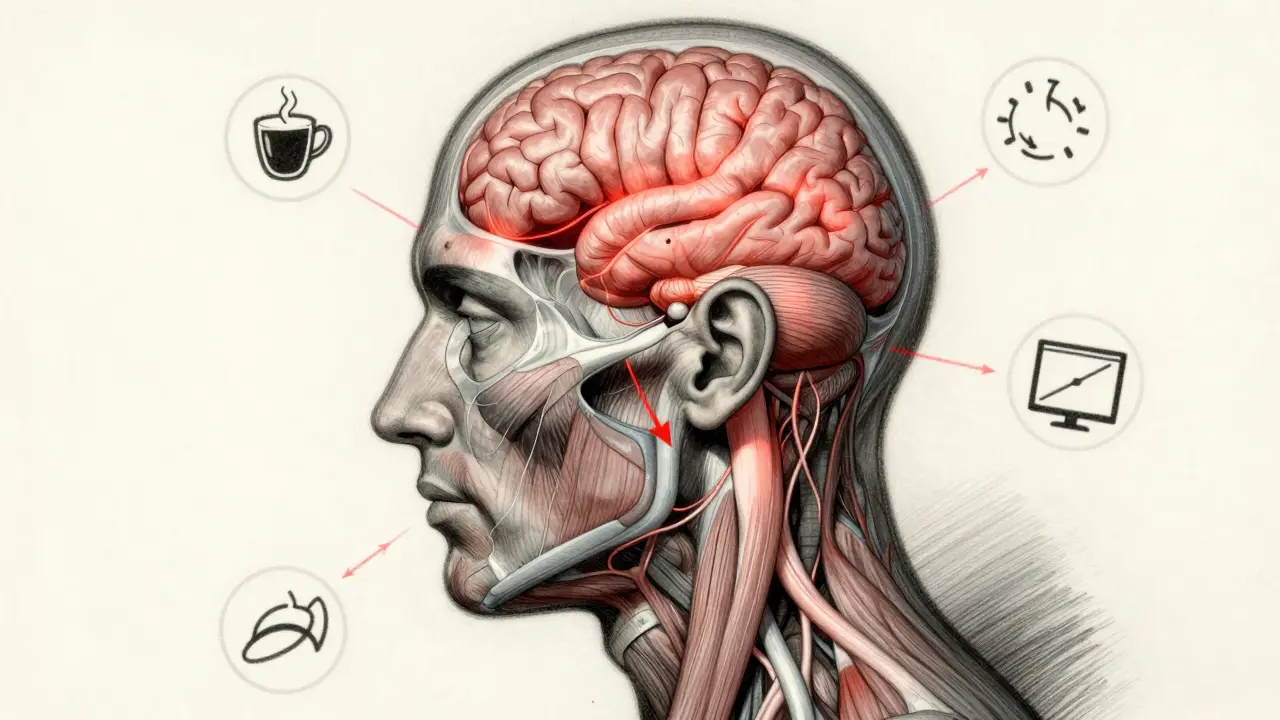
Other triggers? They’re measurable.
- Sleep: Getting less than six hours a night makes you 4.2 times more likely to have a headache.
- Caffeine: If you drink more than 200mg a day (about two cups of coffee) and then skip it, withdrawal hits fast. One day without your usual cup? Headache incoming.
- Screens: More than seven hours a day on devices? You’re 63% more likely to get headaches. It’s not the blue light-it’s the posture. Your head juts forward, straining the muscles at the base of your skull.
- Dehydration: If your blood’s osmolality climbs above 295 mOsm/kg, your brain notices. That’s less than two liters of water a day for most people.
- Medication overuse: Taking painkillers-ibuprofen, paracetamol, even aspirin-more than 10 days a month? You’re not treating the headache. You’re making it worse. This is called medication-overuse headache, and it’s a trap.
And yes, uncorrected vision problems can do it too. If you have astigmatism over 1.5 diopters and read up close for more than 45 minutes without glasses, you’re triggering a headache in nearly 1 in 5 people. It’s not about eye strain-it’s about how your brain processes the effort.
Why Most Treatments Fail (And What Actually Works)
Most people start with the same path: buy ibuprofen. Take it. Feel better. Take it again next time. Then again. Soon, you’re hitting the limit. And then it stops working. That’s not your fault. That’s how the body adapts.
Here’s the reality: acute painkillers are fine for occasional headaches. But if you’re having 15+ headaches a month, you need prevention-not rescue.
Medications That Actually Help
The gold standard for prevention? Amitriptyline. A low-dose tricyclic antidepressant. Sounds odd, right? But it’s been used for decades because it works. Starting at 10mg at night, slowly increasing to 25-50mg, it reduces headache days by 50-70% in six weeks. The catch? Side effects. Dry mouth, weight gain (average 2.3kg), drowsiness. About 1 in 4 people quit because of it.
There’s a better option now: mirtazapine. Also an antidepressant, but with fewer side effects. In a 2022 trial with 187 people, it worked just as well as amitriptyline-but only 35% dropped out, compared to 62% on amitriptyline. It still causes hunger and sleepiness, but less dry mouth and less weight gain.
What doesn’t work? Botulinum toxin (Botox). It’s approved for migraines. Not for tension headaches. And muscle relaxants like cyclobenzaprine? No strong evidence. They make you sleepy. That’s it.
Non-Drug Treatments That Change Everything
Here’s the good news: you don’t have to rely on pills.
- Cognitive Behavioral Therapy (CBT): This isn’t just talking. It’s training your brain to respond differently to pain. Twelve weeks of CBT reduces headache days by 41%. That’s better than most drugs.
- Physical therapy: Not massage. Not cracking your neck. Specific craniocervical flexion exercises-where you gently tuck your chin in while lying down-done for 12 sessions, cut frequency by 53%. Find a physio who specializes in cervicogenic headaches. Only 12% of U.S. physios do.
- Mindfulness: Just 15 minutes a day of focused breathing or body scanning lowers cortisol by 29% in eight weeks. That’s the stress crash you’re trying to avoid.
- Acupuncture: It’s not magic, but it helps. Cochrane Review found it reduces headache days by about 3.2 per month compared to fake acupuncture.
And the 20-20-20 rule? Real. Every 20 minutes, look at something 20 feet away for 20 seconds. It reduces eye strain and neck tension. 83% of people who tried it reported fewer headaches.
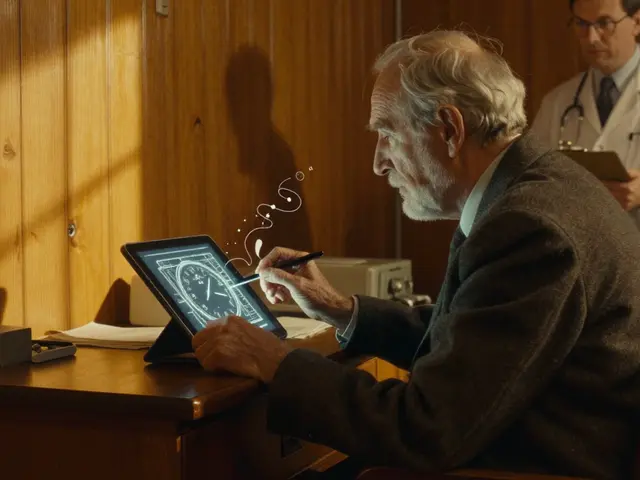
How to Know If You Have It (And What Doctors Miss)
Here’s the problem: doctors are trained to look for red flags-tumors, strokes, infections. But chronic tension headache has no red flags. No abnormal scans. No lab test. Your MRI is normal. Your blood work is fine. So they say, “It’s stress.”
But the real diagnostic tool? Your diary.
Track every headache for three months. Note:
- When it started
- How long it lasted
- What you ate, drank, or did before it hit
- How you slept the night before
- What meds you took
Apps like Migraine Buddy help. But even a notebook works. The goal? Prove you’re having 15+ days a month with tension-type pain. No aura, no vomiting, no light sensitivity.
Doctors miss this diagnosis 38% of the time. They confuse it with chronic migraine. The difference? Migraines hurt on one side, throb, and make you want to hide in a dark room. Tension headaches? They’re dull, everywhere, and you can still function-barely.
What to Avoid (And Why)
Don’t take opioids. They don’t help. They just make you dependent.
Don’t take NSAIDs more than 10 days a month. That’s the line. Cross it, and you’ll get rebound headaches. Nimesulide? Banned in 28 countries for liver damage. Don’t risk it.
Don’t wait until you’re in pain to act. Prevention starts before the headache hits. If you’re having 10 or more headache days a month, you’re already in the prevention zone. Don’t wait for 15.
And don’t believe the myth that tension headaches are harmless. People with chronic tension headaches are 2.1 times more likely to develop depression. It’s not just pain. It’s isolation. It’s burnout. It’s losing your sense of control. That’s why mental health support isn’t optional-it’s part of treatment.

What’s Next? The Future of Treatment
There’s new hope. Atogepant, a drug approved for migraines, is now being tested for chronic tension headaches. Early results show it cuts headache days by over five per month. It’s not approved yet-but it’s in fast-track review.
Researchers are also looking at the gut-brain connection. People with chronic tension headaches have lower levels of a good gut bacteria called Faecalibacterium prausnitzii. Could probiotics help? Maybe. Studies are ongoing.
And nerve stimulation? Tiny devices placed behind the ear to gently stimulate the occipital nerve show promise. In early trials, 62% of users had over half their headaches cut.
By 2027, the next version of the headache classification (ICHD-4) will likely rename chronic tension headache to “primary headache with central sensitization.” That’s not just a name change. It’s science catching up. It’s saying: this isn’t muscle tension. It’s brain wiring.
Real People, Real Results
One person on HealthUnlocked wrote: “I was having 22 headache days a month. I started sleeping at the same time every night-no more than 20 minutes variation. Within three weeks, I was down to nine.”
Another said: “Amitriptyline gave me 8kg weight gain. Switched to mirtazapine. Still hungry, but my headaches dropped by 60%.”
And the most common success story? Consistency. Not magic. Not one fix. Waking up at the same time. Drinking water before coffee. Taking breaks from screens. Doing chin tucks. Not skipping sleep. Not overusing pills.
Chronic tension headache isn’t something you cure. It’s something you manage. But with the right approach, you don’t have to live with it every day. You can take your life back-one small habit at a time.





Comments(14)