Elderly Eczema Moisturizer Recommender
Select Your Skin Conditions
Your Recommended Moisturizer
Living with Eczema is already a daily challenge; add the nuances of aging skin and the game changes. Older adults often see flare‑ups that look like classic eczema, yet the underlying triggers, skin barrier health, and medication tolerances differ from younger patients. This guide walks you through what makes elderly eczema unique, how to pinpoint the cause, and which care plan delivers relief without compromising safety.
Understanding Eczema in Older Adults
When most people hear "eczema," they think of childhood atopic dermatitis. In seniors, the condition is typically labeled as "nummular eczema" or "seborrheic dermatitis," but the core issue-an inflamed, itchy skin barrier-remains the same. The clinical picture may include round, coin‑shaped lesions, crusted patches on the shins, or dry, scaly patches on the scalp. Recognizing these patterns early can prevent chronic scratching and secondary infections.
Why Aging Skin Changes the Game
Age brings three major skin shifts that directly affect eczema management:
- Reduced lipid production: The natural oils that keep skin supple dwindle, weakening the barrier.
- Thinner epidermis: Less collagen means the skin is more fragile and prone to tears.
- Altered immune response: Immune cells become less efficient, shifting the balance between inflammation and repair.
These changes mean that treatments well‑tolerated by younger people can be too harsh for seniors, and moisturizers that work for a teen might feel greasy or cause irritation for an older adult.
Diagnosing Eczema in Seniors
Accurate diagnosis starts with a thorough history and visual exam. Clinicians often use the following steps:
- Ask about symptom onset, flare patterns, and recent changes in soaps, detergents, or clothing.
- Check for comorbidities such as diabetes, peripheral vascular disease, or chronic kidney disease, which can mimic or exacerbate eczema.
- Perform a skin scrape or swab if there’s a suspicion of bacterial or fungal superinfection.
- Consider a patch test when allergens are suspected, especially in cases resistant to standard therapy.
When the diagnosis is uncertain, a dermatologist may order a skin biopsy to rule out psoriasis or skin cancer, both more common in the elderly.
Core Treatment Principles
All successful care plans share three pillars: restore the barrier, calm inflammation, and minimize triggers.
- Moisturizing-the foundation for any eczema regimen.
- Gentle topical steroids or calcineurin inhibitors used sparingly.
- Lifestyle adjustments that reduce sweating, friction, and exposure to irritants.
Below we dive into each pillar with senior‑specific recommendations.
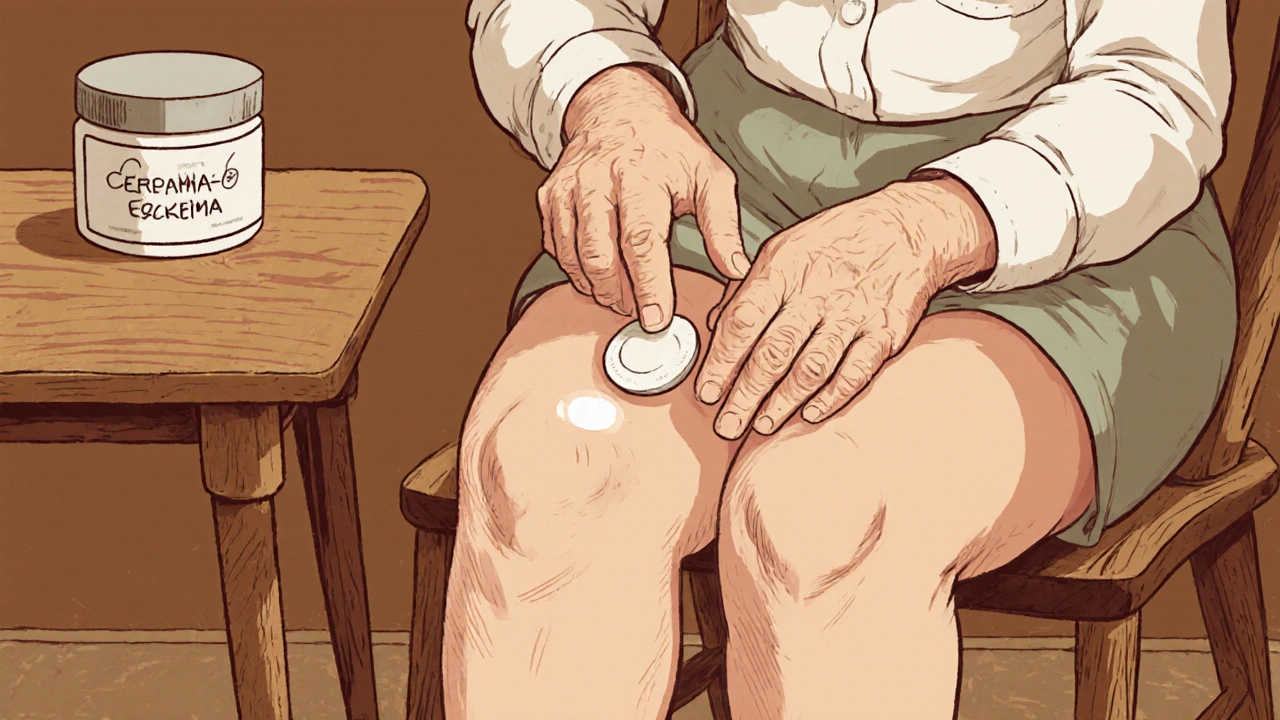
Moisturizing Strategies for Sensitive Aging Skin
Older skin absorbs products quickly, so the choice of moisturizer matters. Look for ointments containing ceramides, cholesterol, and fatty acids-the trio that mirrors the skin’s natural lipid matrix. Avoid fragrances, preservatives like parabens, and high alcohol content, all of which can ignite itching.
| Type | Key Ingredients | Pros for Seniors | Cons |
|---|---|---|---|
| Ointment | Ceramides, petrolatum | Highly occlusive, excellent barrier repair | Greasy feel, may stain clothing |
| Cream | Glycerin, dimethicone | Balanced hydration, easier to spread | Less occlusive than ointments |
| Lotion | Water‑based, hyaluronic acid | Lightweight, quick absorption | May evaporate too fast, less barrier support |
Apply moisturizer immediately after bathing-within three minutes-to lock in moisture. For the elderly, a gentle, lukewarm shower lasting no longer than 10 minutes prevents stripping the skin’s natural oils.
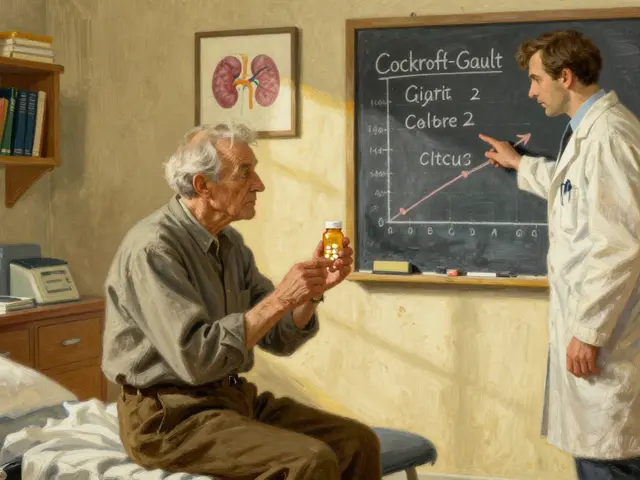
Topical Medications: Benefits and Risks for the Elderly
Topical steroids remain the first‑line anti‑inflammatory agents, but potency must be chosen carefully. Low‑to‑moderate potency (e.g., hydrocortisone 1% or triamcinolone 0.1%) is usually sufficient for thin facial skin, while higher potency creams (e.g., betamethasone dipropionate 0.05%) may be reserved for thick plaques on the elbows or knees, and only for short bursts (7‑10 days).
Long‑term steroid use in seniors raises concerns about skin atrophy, telangiectasia, and systemic absorption that can elevate blood glucose. To mitigate these risks, rotate with calcineurin inhibitors such as tacrolimus ointment 0.1% or pimecrolimus cream 1% for sensitive areas like the eyelids and neck.
Both drug classes should be prescribed with clear instructions: apply a pea‑sized amount, avoid covering with occlusive dressings unless directed, and schedule regular follow‑ups to assess skin response.
When to Consider Light Therapy or Systemic Options
If topical measures fail after a month of consistent use, phototherapy (narrow‑band UVB) can be effective. The elderly often tolerate UVB well because it avoids the systemic side effects of oral steroids, but eye protection is mandatory. Sessions typically last 15‑20 minutes, two to three times per week, with gradual dose escalation.
Systemic immunosuppressants-such as methotrexate, azathioprine, or mycophenolate mofetil-are reserved for severe, refractory cases. Prior to initiation, assess liver function, renal clearance, and potential drug interactions (especially with common senior medications like antihypertensives and anticoagulants). Regular blood monitoring every 4‑8 weeks helps catch toxicity early.

Lifestyle Tweaks and Home Care Tips
Beyond prescription products, everyday habits can tip the balance toward relief:
- Clothing: Choose soft, breathable fabrics (cotton, bamboo) and avoid wool or synthetic blends that can irritate.
- Bath products: Use fragrance‑free, pH‑balanced cleansers. Adding a tablespoon of colloidal oatmeal to bath water soothes itching.
- Hydration: Seniors often have reduced thirst response. Aim for 1.5-2L of water daily unless contraindicated.
- Humidity control: Use a humidifier in winter to keep indoor air at 40‑50% relative humidity, which reduces transepidermal water loss.
- Scratch management: Keep fingernails trimmed short; consider wearing soft cotton gloves at night to block unconscious scratching.
Regular skin checks, especially for signs of infection (pus, increased redness, fever), are vital. Promptly treat bacterial overgrowth with topical antibiotics like mupirocin 2%.
Common Pitfalls and How to Avoid Them
Even well‑intentioned care can backfire. Watch out for these frequent errors:
- Over‑moisturizing: Applying thick ointments under occlusion can create a breeding ground for fungi.
- Skipping patch tests: New detergents or soaps may contain hidden allergens; a simple 48‑hour patch test can spare weeks of flare‑ups.
- Self‑prescribing high‑potency steroids: Without medical guidance, seniors risk skin thinning and systemic effects.
- Neglecting comorbidities: Conditions like diabetes accelerate infection risk; tight glycemic control is part of eczema management.
- Ignoring mental health: Chronic itching can lead to anxiety or depression. Encourage open conversations and consider referral to a therapist if needed.
Addressing these issues early keeps the skin barrier intact and reduces the need for aggressive medication.
Frequently Asked Questions
How often should an elderly person apply moisturizer?
Ideally twice a day-once after a gentle bath and once before bedtime. For very dry skin, a quick mid‑day re‑application can help.
Can over‑the‑counter hydrocortisone be enough?
For mild flare‑ups on non‑sensitive areas, a 1% hydrocortisone cream applied for up to 7 days can be sufficient. If the rash persists, see a clinician for stronger options.
Is phototherapy safe for people over 80?
Yes, when administered under medical supervision. UVB doses start low and are increased gradually. Eye protection and skin cancer screening remain essential.
What dietary changes help eczema in seniors?
A diet rich in omega‑3 fatty acids (salmon, flaxseed), antioxidant vegetables, and low in processed sugars can reduce systemic inflammation, which may calm skin symptoms.
When should I call a doctor for a flare‑up?
If you notice sudden spreading, pus, fever, or if the itching disrupts sleep for more than a few days, seek medical attention promptly.
Managing eczema in the elderly isn’t a one‑size‑fits‑all task. By tailoring moisturizers, choosing the right potency of topical meds, and adjusting daily habits, seniors can keep their skin comfortable and avoid complications. Remember, the best plan combines medical guidance with simple home‑care tweaks-consistency is the real cure.





Comments(11)