When your life changes - whether you’re moving cities, starting a new job, going through a breakup, or caring for a sick relative - your medication routine often gets left behind. Not because you don’t care, but because your brain is overloaded. Stress doesn’t just make you tired. It rewires your habits. And for people managing chronic conditions, that’s dangerous. Research shows medication adherence drops by an average of 32% during major life shifts. That’s not a small slip. That’s a health risk. In fact, 68% of chronic disease flare-ups happen within the first three months after a big change. You’re not failing. Your system just wasn’t built for this.
Why Your Routine Breaks Down During Transitions
It’s not laziness. It’s not forgetfulness. It’s neuroscience. When your life is in flux, your prefrontal cortex - the part that handles planning and decision-making - gets flooded with stress hormones. Suddenly, taking a pill at 8 a.m. feels like one more thing on a list that’s already too long. You’re not alone. On Reddit’s r/ChronicIllness, 78% of users admitted to missing doses during transitions. The top triggers? Relocation (63%), job changes (58%), and relationship shifts (49%). Most apps and pill organizers work fine in stable times. But when your schedule shatters - like after a divorce or a new night-shift job - a simple alarm doesn’t cut it. A 2023 study in the Journal of Medical Internet Research found that while regular reminder apps boost adherence by 23% under normal conditions, that number falls to just 8% during high-stress transitions. Why? Because they don’t adapt. They assume your life stays the same. It doesn’t.The Three Lists: Take Back Control
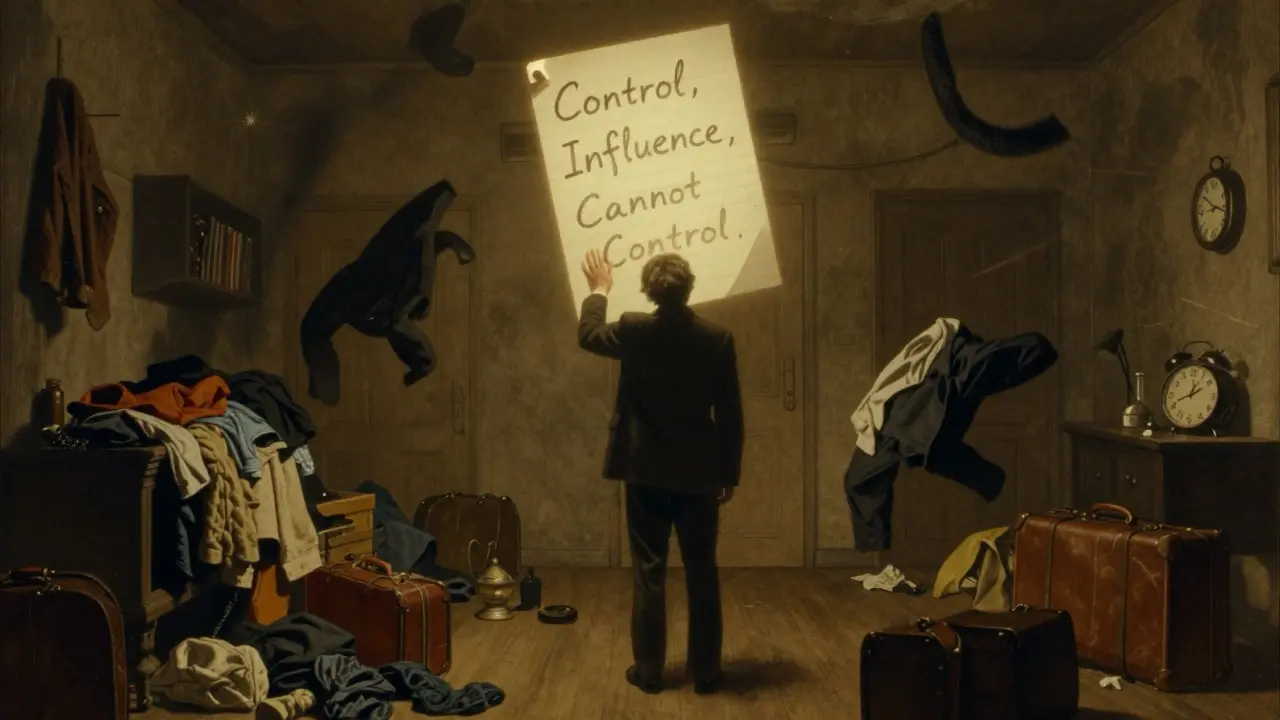
One of the most powerful tools you can use isn’t an app or a pillbox. It’s a piece of paper. Write down three lists:- Things you can control: What time you take your pill, where you keep it, who reminds you.
- Things you can influence: Asking your doctor for a simpler regimen, switching to a once-daily pill, setting up automatic refills.
- Things you can’t control: Your boss’s schedule, your neighbor’s loud party, the pharmacy being out of stock.
Anchor Routines: 3-5 Non-Negotiables
You don’t need to stick to your old schedule. You need anchors. These are small, consistent actions that happen every day - rain or shine, chaos or calm. They’re your emotional ballast. Research from the Journal of Personality and Social Psychology shows that keeping just three to five daily anchors reduces psychological distress by 23% and improves medication adherence by over 31%. What counts as an anchor? Doesn’t matter - as long as it’s consistent. For some, it’s brushing teeth. For others, it’s making coffee, checking the weather, or walking the dog. Pick yours. Then, tie your medication to one of them. Not “take pill at 8 a.m.” - that’s too rigid. Instead: “Take pill after I brush my teeth.” Or “Take pill before I check my email.” Or “Take pill when I sit down for lunch.” This creates habit stacking - a proven behavioral technique. It’s not about the time. It’s about the trigger.
Flexible Time-Blocking Beats Rigid Schedules
Forget alarms that go off at 7:30 a.m. What if you’re working the night shift? What if your kid is sick? What if you’re in a different time zone? Rigid scheduling fails during transitions. Time-blocking doesn’t. Time-blocking means you assign a window - not a minute. Instead of “take pill at 8:00 a.m.,” you say: “I’ll take my pill between 7:30 and 9:30 a.m.” That 2-hour window gives you breathing room. A 2022 study from the Greater Boston Behavioral Health Institute found that this simple shift increased adherence by 28.6% during unstable periods. Why? Because your brain doesn’t panic when things change. You built flexibility into the system.Use the Right Tools - But Not the Ones You Think
Most people reach for apps. But not all apps are equal. General adherence apps like Medisafe or MyTherapy have average ratings of 3.5/5. But tools built for transitions - like TransitionAdhere or LifeShiftRx - score 4.2/5. Why? They ask: “What’s changing?” Then they adapt. Look for features like:- “Change Scenario Planner” - lets you map out how your routine shifts if you move, start a new job, or travel.
- “Flexible Routine Mapping” - lets you drag and drop your meds onto daily anchors instead of fixed times.
- “Emergency Supply Mode” - automatically suggests how to get meds if you’re stuck away from home.
Get Support - But Don’t Wait to Be Asked
Social support isn’t just nice. It’s biological. A 2022 study in Health Psychology found that people who felt supported had 42% lower cortisol levels and 34% better adherence during transitions. But here’s the catch: most doctors don’t ask. Only 23% of providers screened for upcoming life changes in 2020. By 2024, that jumped to 68%. Still not enough. So you have to speak up. Don’t wait for your doctor to notice. Say: “I’m moving next month. How do we make sure I don’t miss doses?” Or: “I just started a new job with unpredictable hours. Can we simplify my regimen?” You can also lean on friends or family. Not to nag you - but to help you design the system. Ask someone: “Can you help me figure out where to keep my pills at my new place?” Or: “Can you remind me to refill my prescription next week?” That’s not burdening them. That’s building a team.
Therapy Works - Especially Acceptance and Commitment Therapy
If you’re struggling emotionally - if you feel overwhelmed, guilty, or hopeless about your meds - therapy isn’t optional. It’s essential. A 2022 JAMA Internal Medicine trial found that Acceptance and Commitment Therapy (ACT) improved adherence by 48.6% during transitions. That’s more than double the effect of standard counseling. ACT doesn’t try to “fix” your stress. It teaches you to sit with it - and still take your pill. It helps you say: “I’m anxious about this move. And I’m still taking my medication.” That’s the breakthrough. You don’t need to feel okay to do what’s right. You just need to know you can do it anyway.What to Do Right Now
You don’t need to overhaul your life. Start with one step today:- Grab a notebook. Write your three lists: control, influence, cannot control.
- Pick one daily anchor - something you already do. Tie your medication to it.
- Check your pill app. Does it let you adjust times? If not, switch to one that does.
- Call your doctor. Say: “I have a big change coming. Can we make my plan more flexible?”
- Text one person: “I need your help with my meds next month. Can we talk?”
What Providers Should Do (And What You Can Push For)
The system is catching up. The American College of Physicians now recommends screening for life transitions at every appointment. The FDA is drafting guidelines. Hospitals are starting to track transition-related readmissions. But you can’t wait for them to fix it. Ask for:- A transition-specific adherence plan - not just a refill reminder.
- Longer prescriptions (90-day fills) to avoid pharmacy disruptions.
- Mail-order or home delivery options.
- A simple, once-daily regimen if possible.
- A referral to a behavioral health specialist if you’re feeling overwhelmed.
Life transitions aren’t exceptions. They’re the norm. You’ll move. You’ll change jobs. You’ll lose someone. You’ll gain new responsibilities. Your health plan should grow with you - not collapse when you do. The goal isn’t perfection. It’s continuity. One pill. One anchor. One conversation. That’s how you stay on track when everything else is falling apart.
Why do I miss my meds during big life changes even though I care about my health?
It’s not about motivation - it’s about cognitive load. When your brain is overwhelmed by change - moving, job loss, divorce - your ability to maintain routines drops. Stress hormones shut down the parts of your brain responsible for planning. You’re not lazy. Your system is overloaded. The solution isn’t to try harder. It’s to redesign your routine to fit the new chaos.
Are reminder apps useless during transitions?
Not useless - but limited. Standard reminder apps work well in stable environments, improving adherence by about 23%. But during major transitions, that benefit drops to just 8%. Why? Because they don’t adapt. They assume your schedule stays the same. You need apps that let you map your meds to daily anchors - not fixed times - and adjust when your life shifts.
What’s the difference between “control” and “influence” in the three-list method?
“Control” means you can directly do it: take your pill at a certain time, set an alarm, keep your meds in your bag. “Influence” means you can change the system: ask your doctor for a once-daily pill, switch to mail-order pharmacy, request a 90-day supply. You can’t control the pharmacy running out - but you can influence it by ordering early. Focusing energy on these two areas reduces stress and boosts adherence.
How long does it take to build a transition-proof medication routine?
Most people see improvement within 2-3 weeks of starting a transition-specific plan. Initial setup takes 4-6 hours: mapping your anchors, choosing the right app, talking to your doctor, writing your lists. The key is not perfection - it’s consistency. Even one solid anchor tied to your meds can make a big difference.
Can therapy really help me take my pills during stress?
Yes - especially Acceptance and Commitment Therapy (ACT). A 2022 study found ACT improved adherence by 48.6% during transitions. It doesn’t make stress disappear. It teaches you to take your pill even when you feel overwhelmed, anxious, or guilty. That’s the power: you don’t need to feel okay to do what’s right. You just need to know you can.
What should I ask my doctor about upcoming life changes?
Say: “I’m going through a big change soon - [moving, starting a new job, etc.]. Can we make my medication plan more flexible? Can I get a 90-day supply? Can we switch to a once-daily pill? Can you help me set up mail-order delivery?” Most providers now screen for transitions. You’re not being difficult - you’re being smart.
Next steps: Start with one anchor. One list. One conversation. That’s how you protect your health when life gets messy.





Comments(14)