Hydroxyurea vs. Alternatives Comparison Tool
Select a therapy to compare its features with Hydroxyurea:
Choose a therapy to see detailed comparison
Hydroxyurea is a ribose analog that inhibits ribonucleotide reductase, slowing DNA synthesis and reducing cell proliferation. It’s sold under the brand name Hydrea and is FDA‑approved for sickle cell disease (SCD), polycythemia vera (PV), and several myeloproliferative neoplasms (MPNs).
Why Patients Reach for Hydroxyurea
Hydroxyurea works by increasing fetal hemoglobin (HbF) in red blood cells, which makes them less likely to sickle. In PV, it curbs the over‑production of red cells, decreasing blood viscosity. Clinical trials from the early 1990s reported a 30‑40% drop in vaso‑occlusive crises for SCD and a 20% reduction in thrombotic events for PV.
Key attributes of Hydroxyurea:
- Oral dosing: usually 15-35mg/kg/day for SCD, 15‑20mg/kg/day for PV.
- Half‑life: 2-5hours, allowing once‑daily administration.
- Primary side‑effects: myelosuppression, renal toxicity, teratogenicity.
Major Safety Considerations
Because Hydroxyurea suppresses the bone marrow, regular blood count monitoring is mandatory. A typical schedule is CBC every 4weeks for the first three months, then every 8-12weeks once stable. Renal function should be checked quarterly, especially in patients with baseline kidney disease. Pregnancy is a strict contraindication; the drug is classified as Category D.
Alternative Therapies in the Same Indication Space
Over the past decade, several newer agents have entered the market. They differ in mechanism, administration route, and side‑effect profile. Below are the most frequently discussed alternatives.
L‑glutamine is a conditionally essential amino acid that reduces oxidative stress in sickle cells. Approved in 2017 for SCD, it’s taken twice daily at 0.3g/kg.
Voxelotor is a hemoglobin‑oxygen affinity modulator that stabilizes the oxygenated form of HbS. FDA‑approved in 2019, typical dose is 1500mg once daily.
Crizanlizumab is a monoclonal antibody targeting P‑selectin, preventing cell‑cell adhesion that triggers vaso‑occlusion. Administered intravenously at 5mg/kg every 2weeks.
Interferon‑alpha is a cytokine that modulates immune response and reduces clonal proliferation in MPNs. Subcutaneous injection, 3‑6million IU thrice weekly.
Ruxolitinib is a JAK1/2 inhibitor that blocks signaling pathways driving myeloproliferation. Oral tablet, 10‑25mg twice daily for PV or essential thrombocythemia.
Side‑Effect Snapshot of the Alternatives
- L‑glutamine: mild gastrointestinal upset, rare liver enzyme elevations.
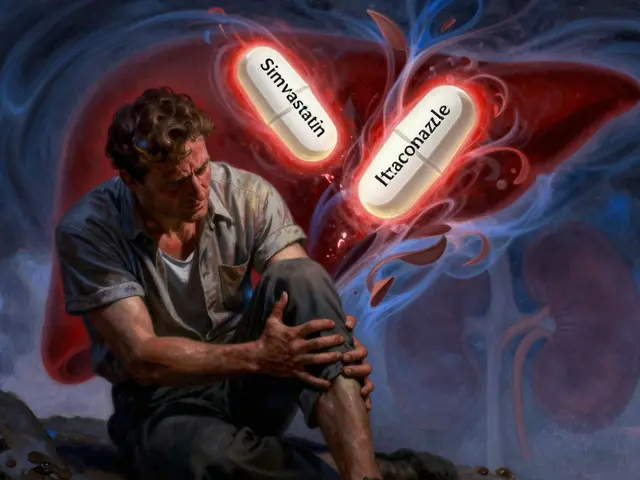
- Voxelotor: headache, increased bilirubin, potential liver toxicity.
- Crizanlizumab: infusion‑related reactions, mild hypertension.
- Interferon‑alpha: flu‑like symptoms, depression, thyroid dysfunction.
- Ruxolitinib: anemia, thrombocytopenia, increased infection risk.
How the Options Stack Up - Comparison Table
| Drug | Indication(s) | Mechanism | Route | Key Side‑Effects | Typical Dose |
|---|---|---|---|---|---|
| Hydroxyurea | SCD, PV, MPNs | Ribonucleotide reductase inhibition → ↑ HbF, ↓ cell proliferation | Oral | Myelosuppression, renal toxicity, teratogenic | 15‑35mg/kg/day (SCD); 15‑20mg/kg/day (PV) |
| L‑glutamine | SCD | Reduces oxidative stress in erythrocytes | Oral | GI upset, rare liver enzyme rise | 0.3g/kg twice daily |
| Voxelotor | SCD | Stabilizes oxygenated HbS | Oral | Headache, bilirubin increase | 1500mg daily |
| Crizanlizumab | SCD | P‑selectin blockade → ↓ vaso‑occlusion | IV | Infusion reactions, hypertension | 5mg/kg every 2weeks |
| Interferon‑alpha | MPNs (incl. PV) | Immune modulation, anti‑proliferative | Sub‑Q | Flu‑like, depression, thyroid issues | 3‑6millionIU thrice weekly |
| Ruxolitinib | PV, essential thrombocythemia | JAK1/2 inhibition → ↓ cytokine signaling | Oral | Anemia, thrombocytopenia, infections | 10‑25mg twice daily |
When Hydroxyurea Still Wins
If you need a low‑cost, oral, once‑daily option with decades of real‑world safety data, Hydroxyurea remains the go‑to. It’s especially attractive for patients who cannot tolerate injections (Crizanlizumab) or who have limited insurance coverage for biologics.
Guidelines from the American Society of Hematology (2023) still list Hydroxyurea as first‑line for both SCD and high‑risk PV. The drug’s ability to reduce stroke risk in children with SCD is unmatched by any newer oral agent.
When to Switch or Add an Alternative
Consider a switch when any of these happen:
- Persistent myelosuppression despite dose adjustments.
- Renal impairment (eGFR<30mL/min/1.73m²) that heightens toxicity risk.
- Inadequate clinical response after 6months at maximally tolerated dose.
- Patient preference for less frequent monitoring (e.g., IV Crizanlizumab every 2weeks).
Combination therapy is an emerging strategy: Hydroxyurea plus L‑glutamine or Voxelotor can provide additive reduction in crisis frequency while keeping each drug at a lower dose.
Cost and Access Snapshot
Hydroxyurea generic versions average $0.10‑$0.25 per 500mg tablet in the U.S., making it affordable for most insurance plans. By contrast, Crizanlizumab can exceed $30,000 per year, and Voxelotor hovers around $10,000‑$12,000 annually. Interferon‑alpha and Ruxolitinib sit in the mid‑range ($5,000-$7,000). These cost differences often drive the decision in resource‑limited settings.
Related Concepts and Next Steps
Understanding Hydroxyurea’s role links to broader topics such as myeloproliferative neoplasms, hemoglobinopathies, and targeted therapy development. Readers interested in the genetics behind sickle‑cell disease may explore gene‑editing approaches like CRISPR‑Cas9, while those focusing on PV might dive into JAK2 V617F mutation testing.
Future articles could cover:
- Gene therapy updates for sickle cell disease.
- Long‑term safety data on JAK inhibitors in PV.
- Nutrition and lifestyle measures that complement pharmacotherapy.

Frequently Asked Questions
Can Hydroxyurea be used in children with sickle cell disease?
Yes. Pediatric trials show that Hydroxyurea reduces vaso‑occlusive events and acute chest syndrome in children as young as 9months. Dosing starts low (around 15mg/kg/day) and is titrated to the maximum tolerated dose while monitoring blood counts every 4weeks.
What monitoring is required while on Hydroxyurea?
Baseline CBC, renal panel, and liver enzymes are essential. After initiation, CBC should be checked every 2‑4weeks until stable, then every 8‑12weeks. Renal function is reviewed quarterly. Pregnancy tests are mandatory for women of child‑bearing potential.
Is Hydroxyurea safe during pregnancy?
No. Hydroxyurea is teratogenic and classified as Category D. Women should discontinue the drug at least three months before attempting conception and discuss alternative therapies with their hematologist.
How does Voxelotor differ from Hydroxyurea?
Voxelotor directly increases hemoglobin’s affinity for oxygen, preventing sickling at the molecular level. Hydroxyurea works indirectly by raising HbF. Voxelotor does not cause myelosuppression but can raise bilirubin levels and is more expensive.
When is Ruxolitinib preferred over Hydroxyurea in polycythemia vera?
Ruxolitinib is usually reserved for patients who have failed or are intolerant to Hydroxyurea, especially those with severe thrombocytosis or splenomegaly. Its JAK1/2 inhibition provides better control of splenic size and systemic symptoms.





Comments(16)